Cerebral desaturations: Know the risks - and the solutions

Edwards Lifesciences Critical Care product group is now part of BD (Becton, Dickinson and Company). Edwards is the manufacturer of the products.
To find the latest information, please visit this page on BD.com
Cerebral desaturations – common, critical and treatable
Research has consistently shown that cerebral tissue oxygen desaturations are common across a broad spectrum of surgical procedures and patient populations – and that they can cause significant complications when left untreated, including:
- Increased hospital & ICU length of stay (LOS)
- Increased incidence of POCD
- Decreased survival
By understanding the incidence, risks and interventions available to address them, you may be able to identify – and even reverse – cerebral desaturations.
Incidence and impact of cerebral desaturations
The cardiac surgical population in particular has demonstrated a significant incidence of cerebral desaturations, which has been associated with a wide range of adverse outcomes.1-9



Read more about risks and outcomes of cerebral desaturations
Preserve brain health: understand and intervene
Detecting, preventing and avoiding cerebral desaturations are critical in helping to assure patient brain health.
While desaturations can lead to serious complications, the good news is that with the right interventions at the right time, they can be treated – and even reversed.

Reversing desaturations can improve outcomes
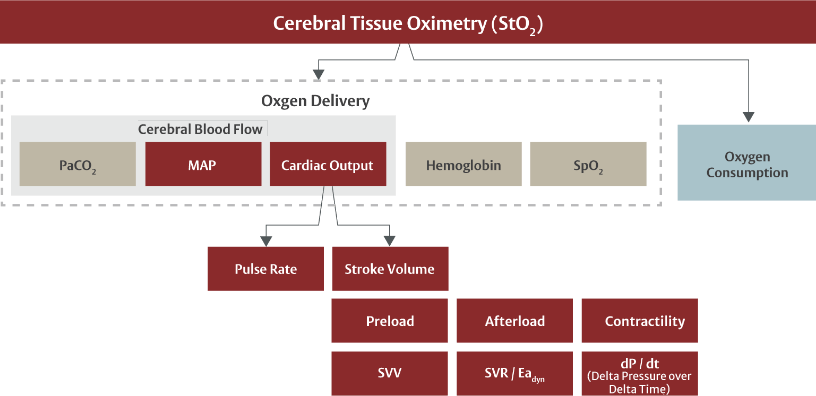
Cerebral desaturations result from an imbalance in the brain tissue’s oxygen consumption and delivery.
Mitigating desaturations depends on an understanding of the various physiologic factors that impact this balance.
This graphic summarizes interventions that have been shown to increase StO2.
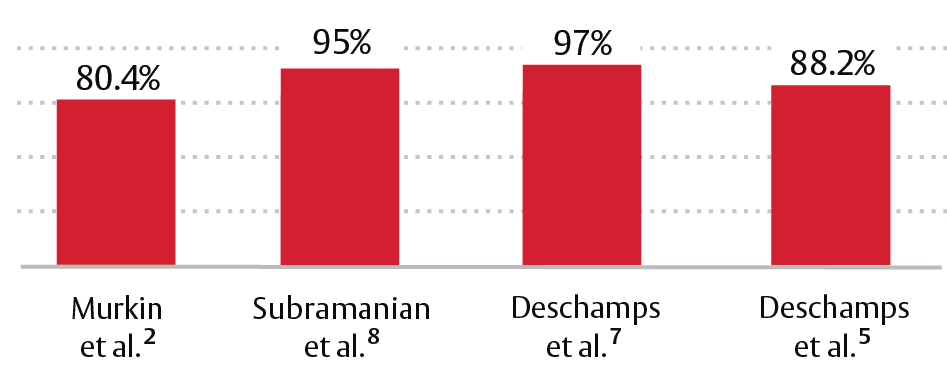
Success of interventions to reverse cerebral desaturations
Watch: Physiologic factors affecting cerebral brain health
For an in-depth look at these physiologic factors and how they impact brain tissue oxygenation (StO2) values, explore this video.
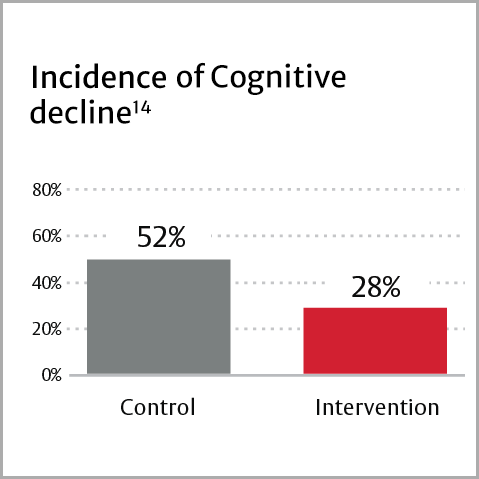
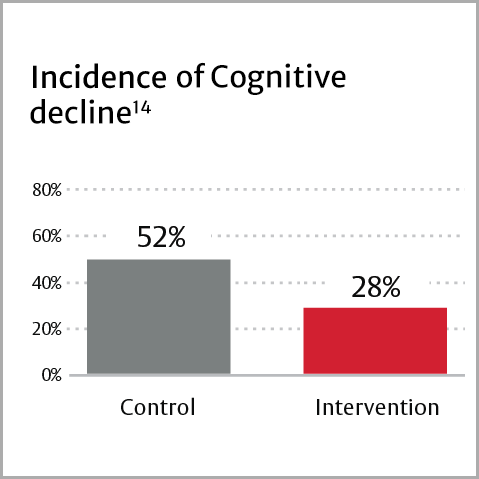
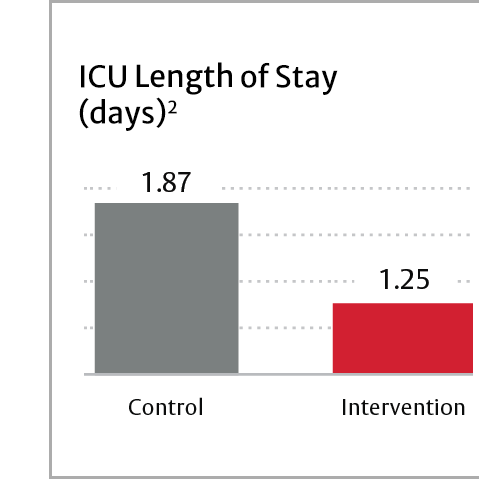
Reversing or avoiding cerebral desaturations has been shown to lead to:
- Reduced incidence of cognitive impairment
- Reduced ICU stay
- Reduced hospital stay
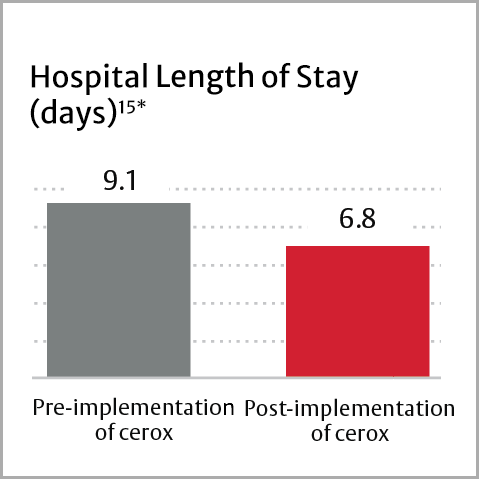
*NYHA class 1
Intervene with confidence – tissue oximetry

Cerebral oximetry is the only technology that monitors cerebral oxygenation noninvasively and continuously – allowing clinicians to detect imbalances and optimize perfusion to avoid and even reverse adverse outcomes.
By using StO2 in conjunction with vital signs, advanced hemodynamic monitoring and laboratory assessments, clinicians can identify the root cause of imbalances and intervene appropriately.
The ForeSight system difference
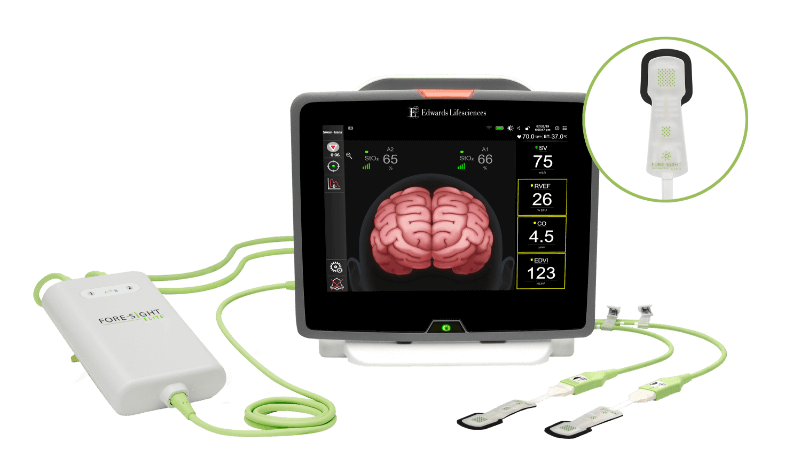
A complete, individualized view of tissue oximetry is key to treating or reversing desaturations – but not all monitoring systems deliver these critical insights.
Some systems are not designed to account for differing patient anatomies, do not give clear, reliable oxygen saturation measures, or do not indicate the root cause of desaturations.
ForeSight sensor offers a unique design and exclusive fifth wavelength of near infrared light (NIRS), to account for these patient differences – enabling reliable StO2 measures from patient to patient.
Only the ForeSight tissue oximetry system:
- Accounts for individual differences, including skin tone, size, age, skin-to-cortex distance and acuity
- Delivers absolute StO2 values, making preinduction baselines optional
- Integrates with the HemoSphere platform for an all-in-one view of patient perfusion
See the complete picture of oxygen delivery and consumption
Treating and avoiding cerebral desaturations depends on a comprehensive view of hemodynamics.
That’s why ForeSight sensor integrates with HemoSphere monitor, delivering advanced parameters like cardiac output (CO) and mean arterial pressure (MAP) – and displays these insights on a single monitor.
This “all-in-one” view delivers comprehensive insights into hemodynamics that can help you drill down to identify the root cause of imbalances – enabling you to administer interventions with confidence.
*PaCO2, Hgb, SpO2 not currently available on HemoSphere monitor
Edwards clinical education
Comprehensive education empowering clinical advancement
With a long-term commitment to improving the quality of care for surgical and critical care patients through education, Edwards clinical education meets you no matter where you are in the learning process – with a continuum of resources and tools that continuously support you as you solve the clinical challenges facing you today, and in the future.
References
- Yao FSF, et al. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18(5):552-558.
- Murkin JM, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104(1):51-58.
- Schön J, et al. Cerebral oxygen saturation monitoring in on-pump cardiac surgery – A 1 year experience. Appl Cardiopulm Pathophysiol. 2009;13: 243-252.
- de Tournay-Jetté, et al. The relationship between cerebral oxygen saturation changes and postoperative cognitive dysfunction in elderly patients after coronary artery bypass graft surgery. Cardiothorac Vasc Anesth. 2011;25(1):95-104.
- Deschamps A, et al. Reversal of decreases in cerebral saturation in high-risk cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(6):1260-1266.
- Greenberg SB, et al. Cerebral desaturation events in the intensive care unit following cardiac surgery. J Crit Care. 2013;28(3):270-276.
- Deschamps A, et al. Cerebral oximetry monitoring to maintain normal cerebral oxygen saturation during high-risk cardiac surgery: a randomized controlled feasibility trial. Anesthesiology. 2016;124(4):826-836.
- Subramanian B, et al. A multicenter pilot study assessing regional cerebral oxygen desaturation frequency during cardiopulmonary bypass and responsiveness to an intervention algorithm. Anesth Analg. 2016;122(6):1786-1793.
- Uysal S, et al. Optimizing cerebral oxygenation in cardiac surgery: A randomized controlled trial examining neurocognitive and perioperative outcomes. J Thorac Cardiovasc Surg. 2020;159(3):943-953.
- Slater JP, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87(1):36-45.
- Stannard, B., Levin, M. A., Lin, H. M., & Weiner, M. M. (2021). Regional cerebral oximetry is consistent across self-reported racial groups and predicts 30-day mortality in cardiac surgery: a retrospective analysis. J Clin Monit Comput. 35(2), 413–421.
- Hong SW, et al. Prediction of cognitive dysfunction and patients’ outcome following valvular heart surgery and the role of cerebral oximetry. Eur J Cardiothorac Surg. 2008;33(4):560-565.
- Fischer GW, et al. Noninvasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg. 2011;141(3):815-821.
- Colak Z, et al. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery: a randomized, prospective study. Eur J Cardiothorac Surg. 2015;47(3):447-54.
- Goldman S, et al. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7(5):E376-81.
Important safety information
Important safety information
CAUTION: Federal (United States) law restricts this device to sale by or on the order of a physician.
See Instructions For Use (IFU) / Directions For Use (DFU) for full prescribing information, including indications, contraindications, warnings, precautions and adverse events.



