Behind your patients, ahead of aortic regurgitation

Getting AR patients the care they need
Aortic regurgitation (AR) is the third most common valvular pathology found in the general population, with a lifetime risk of 13% in men and 8.5% in women.1
It is critical to diagnose and treat AR early, as progression is associated with increased mortality risk. Within ten years of diagnosis of severe AR, 75% of patients die or require aortic valve replacement.1-4
Cardiologists play a key role in identifying AR and getting patients the care they need before it's too late.
AR prevalence increases with age
The Framingham Heart Study (1999) was a prospective epidemiological study that included the evaluation of the prevalence and severity of AR by color Doppler examination performed between 1991 and 1995.5
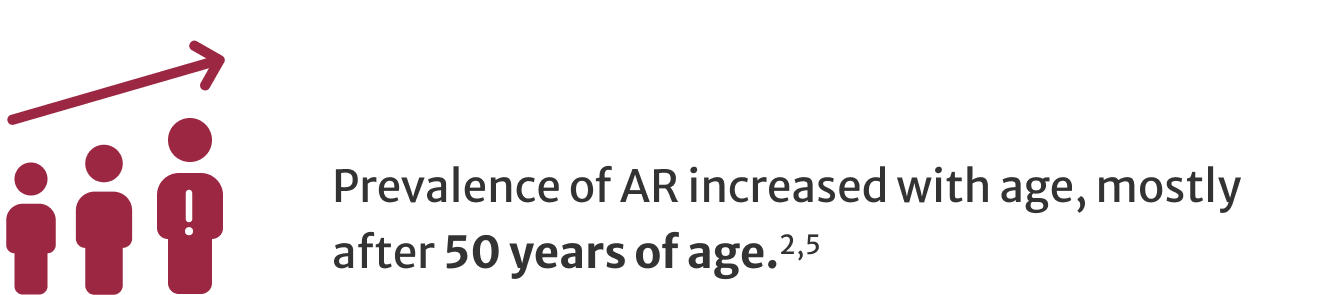
Progression of AR can be variable and exponentially increases mortality risk.2,3
Rates of progression are determined by a complicated interaction of several variables, including AR severity, aortic root pathology, and the adaptive response of the left ventricle (LV).6
Intervention is key to patient outcomes
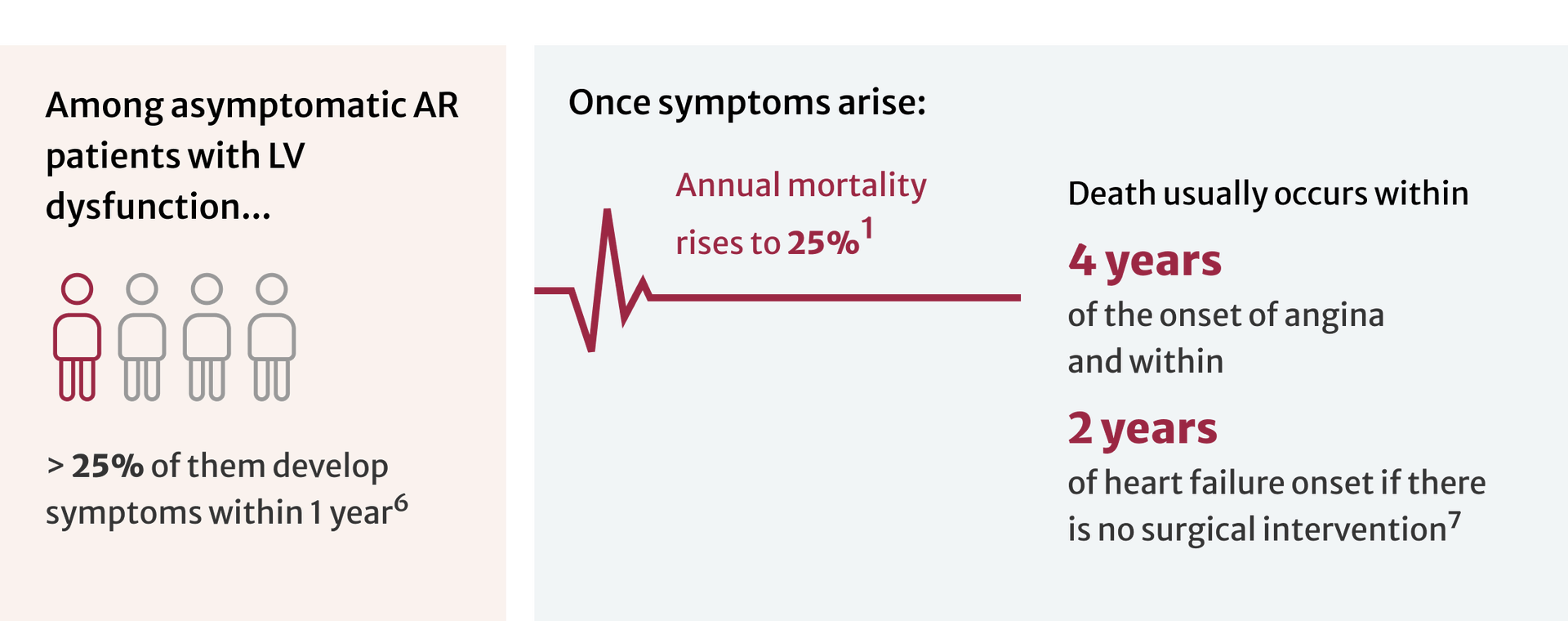
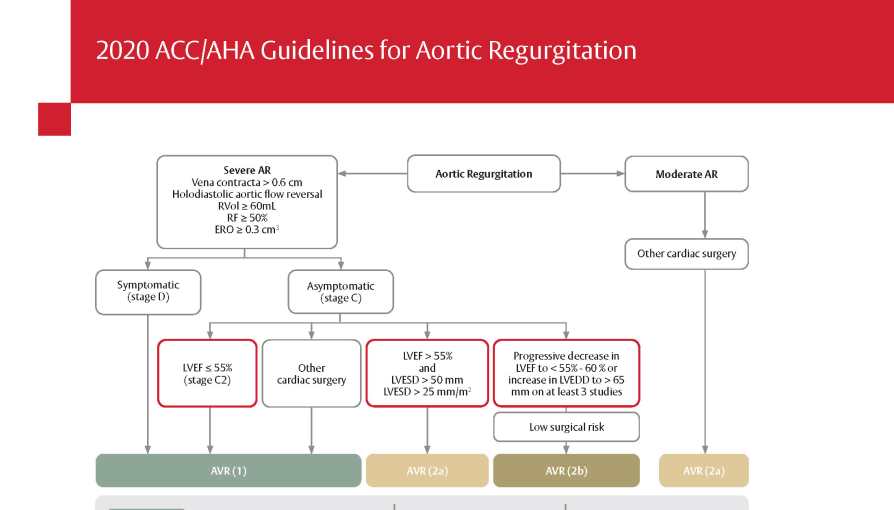
According to guidelines from the American College of Cardiology (ACC)/American Heart Association(AHA), European Society of Cardiology (ESC), and Japan Circulation Society (JCS), surgery is indicated in symptomatic severe AR regardless of LV function.
Timely Evaluation for Surgical Treatment of Aortic Valve Disease

Timely Evaluation for Surgical Treatment of Aortic Valve Disease

Relying on symptoms alone may result in an intervention with poorer outcomes3,8
Even in asymptomatic severe AR, mortality can be as high as 19% within 6.6 years of diagnosis.1
Current U.S. and European guidelines recommend surgical intervention before symptoms develop in severe AR patients with LV dysfunction, primarily based on echocardiographic parameters.9,10
2020 ACC/AHA Guidelines for Aortic Regurgitation
2020 ACC/AHA Guidelines for Aortic Regurgitation
Echocardiography is the initial method of AR evaluation9-11
Video provided courtesy of Jordan B. Strom, MD, MSc, FACC, FASE, Director, Echocardiography Laboratory, Division of Cardiovascular Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA, January 2023
Multiple echocardiographic parameters are required to precisely quantify AR.11 Transthoracic echocardiography (TTE) is an essential first diagnostic test, and measurements obtained are frequently sufficient to evaluate the presence and severity of AR.9, 11

Echocardiography allows for the:
- Assessment of the motion of aortic leaflets and anatomy of the aortic root
- Detection of the presence and severity of AR
- Characterization of LV size and function11
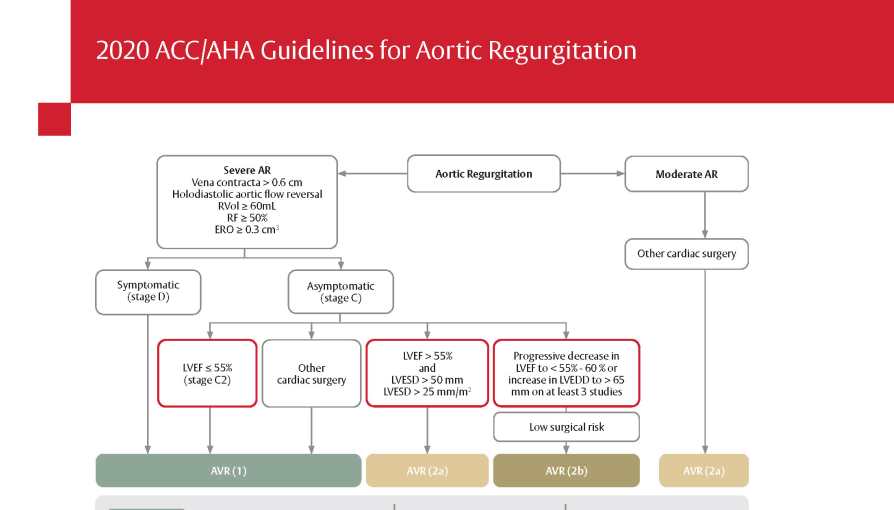
An analysis of severe symptomatic AR (ssAR) patients and mortality
In an analysis of the Optum database from 2008-2016:
- Despite the class 1 indication for SAVR, most patients with ssAR do not receive treatment within one year12
- A patient’s primary cardiologist was a strong determinant of likelihood of receiving SAVR, particularly for patients with reduced LVEF12


Clinical summary: Treatment patterns, disparities, and management strategies impact clinical outcomes in patients with symptomatic severe aortic regurgitation
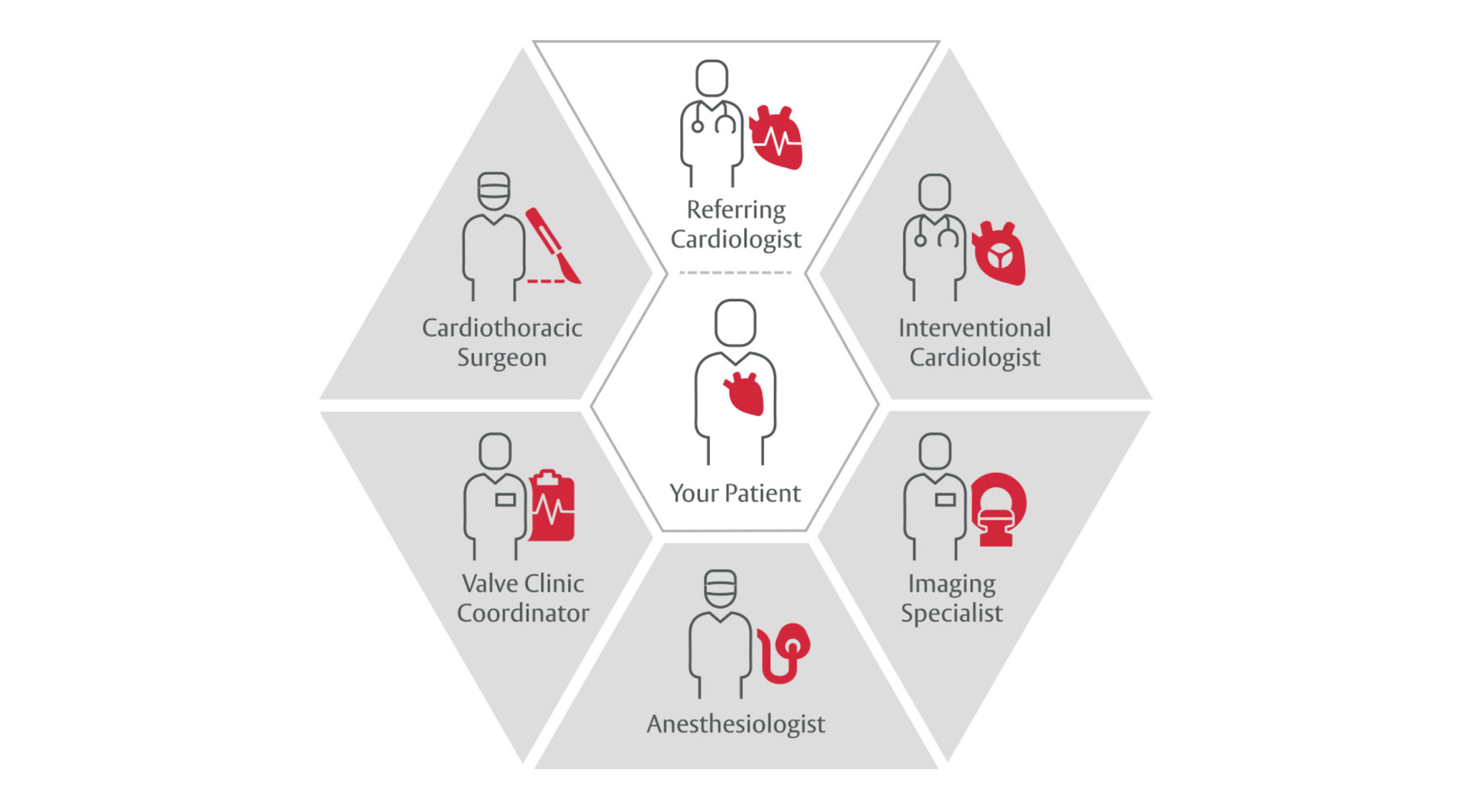
The Heart Team builds on the foundation of the care you provide
All patients with severe valvular heart disease being considered for valve intervention should be evaluated by a multidisciplinary team with either referral to or consultation with a primary or comprehensive valve center.9
Help your patients understand aortic regurgitation
What it is, symptoms to look for, and available treatments.
Understanding Aortic Regurgitation

Understanding Aortic Regurgitation

References
- Galusko V, Thornton G, Jozsa C, et al. Aortic regurgitation management: a systematic review of clinical practice guidelines and recommendations. Eur Heart J Qual Care Clin Outcomes. 2022;8(2):113-126.
- Akinseye OA, Pathak A, Ibebuogu UN. Aortic valve regurgitation: a comprehensive review. Curr Probl Cardiol. 2018;43(8):315-334.
- Wang SS. Aortic Regurgitation. The heart.org and Medscape. https://emedicine.medscape.com/article/150490-overview. Updated December 7, 2021.
- Flint N, Wunderlich, N, Shmueli, H, et al. Aortic regurgitation. Curr Cardiol Rep. 2019;21:65.
- Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999;83(6):897–902.
- Bekeredjian R, Grayburn PA. Valvular heart disease. Circulation. 2005;112(1):125–34.
- Aksoy O, Griffin BP. Aortic Valve Disease. In: Valvular heart disease. 4th ed. Manual of Cardiovascular Medicine, vol1. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. p. 259.
- Yang LT, Michelena HI, Scott CG, et al. Outcomes in Chronic Hemodynamically Significant Aortic Regurgitation and Limitations of Current Guidelines. J Am Coll Cardiol. 2019;73(14):1741-1752.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline. Circulation. 2021;143(5):e35-e71.
- Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines. Euro Heart J. 2022; 43(7):561-632.
- Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30(4):303-371.
- Thourani VH, Brennan MJ, Edelman JJ, et al. Treatment Patterns, Disparities, and Management Strategies Impact Clinical Outcomes in Patients with Symptomatic Severe Aortic Regurgitation. Structural Heart 2021; 5(6): 608-618.