参考文献
- 美国急救医师学会(ACEP)脓毒症专家小组。 DART证据驱动工具指南。
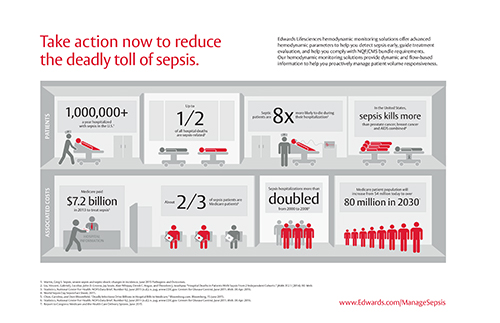
- Statistics, National Center For Health. NCHS Data Brief, Number 62, June 2011 (n.d.): n. pag. www.CDC.gov . Centers for Disease Control, June 2011. Web. 6 Apr. 2016.
- Liu, Vincent, Gabriel J. Escobar, John D. Greene, Jay Soule, Alan Whippy, Derek C. Angus, and Theodore J. Iwashyna. "Hospital Deaths in Patients With Sepsis From 2 Independent Cohorts." Jama 312.1 (2014): 90. Web.
- Statistics, National Center For Health. NCHS Data Brief, Number 62, June 2011 (n.d.): n. pag. www.CDC.gov . Centers for Disease Control, June 2011. Web. 6 Apr. 2016.
- World Sepsis Day Sepsis Fact Sheet, 2015.
- Marik, Paul E., Xavier Monnet, and Jean-Louis Teboul. 揌emodynamic Parameters to Guide Fluid Therapy.? Ann Intensive Care Annals of Intensive Care 1.1 (2011):1. Web.
- Martin, Greg S. 揝epsis, Severe Sepsis and Septic Shock: Changes in Incidence, Pathogens and Outcomes.? Expert review of anti-infective therapy 10.6 (2012): 701–706. PMC. Web. 12 July 2016.
- Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006.
- Truijen et al. Noninvasive Continuous Hemodynamic Monitoring. Journal of Clinical Monitoring and Computing. 2012.
- 操作手册EV1000_157811A5。
- EV1000操作手册(S-0351)。
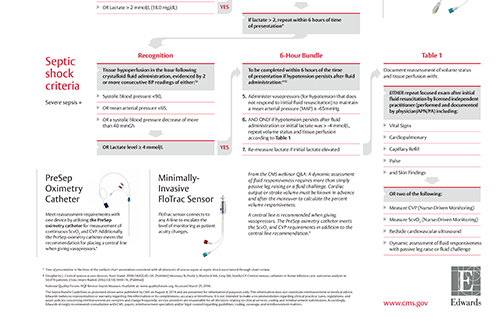
- 政府: 脓毒症集束治疗项目- SEP1。
- Eeftinck Schattenkerk D, et al. Nexfin Noninvasive Continuous Blood Pressure Validated Against Riva-Rocci/Korotkoff. American Journal of Hypertension 2009; 22(4):378-383.
- Maguire S, et al. Respiratory Variation in Pulse Pressure and Plethysmographic Waveforms: Intraoperative Applicability in a North American Academic Center. Anesthesia & Analgesia 2011;112:94-6.
- Dougherty L. Central venous access devices. Nurs Stand. 2000;14(43):45-50. [PubMed]
- Moureau N, Poole S, Murdock MA, Gray SM, Semba CP. Central venous catheters in home infusion care: outcomes analysis in 50,470 patients. J Vasc Interv Radiol. 2002;13(10):1009-16. [PubMed]
- Reinhart K, et al. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30(8):1572-8.
- Rivers EP, et al. Central venous oxygen saturation monitoring in the critically ill patient. Curr Opin Crit Care. 2001;7(3):204-11.
- Ingelmo P, et al. Importance of monitoring in high risk surgical patients. Minerva Anestesiol. 2002;68(4):226-30.
- Scalea, TM, et al. Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma 1990;30(12):1539-43.
- Ander, DS, et al. Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 1998;82(7):888-91.
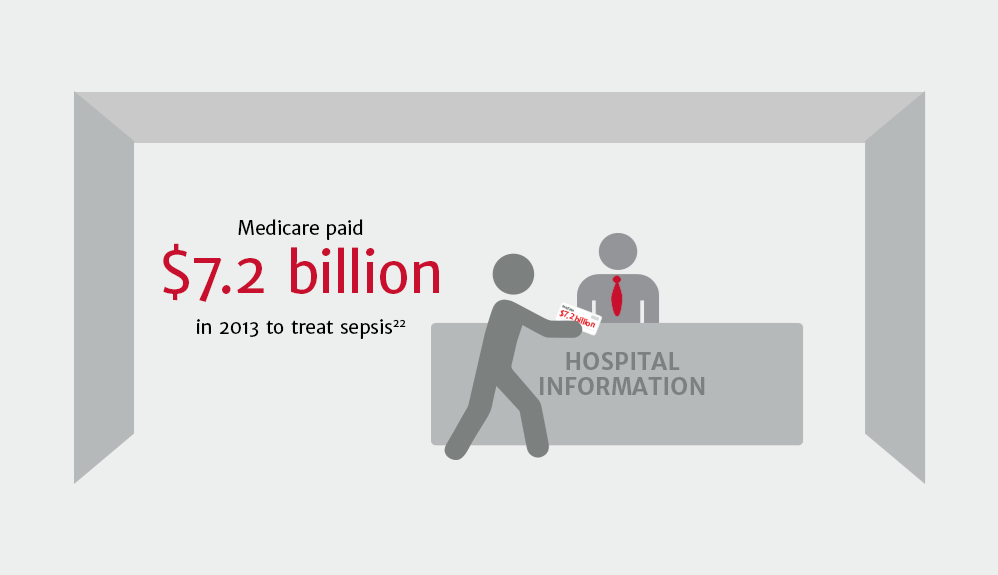
- Chen, Caroline, and Doni Bloomfield. "Deadly Infections Drive Billions in Hospital Bills to Medicare." Bloomberg.com . Bloomberg, 15 June 2015. Web. 06 Apr. 2016
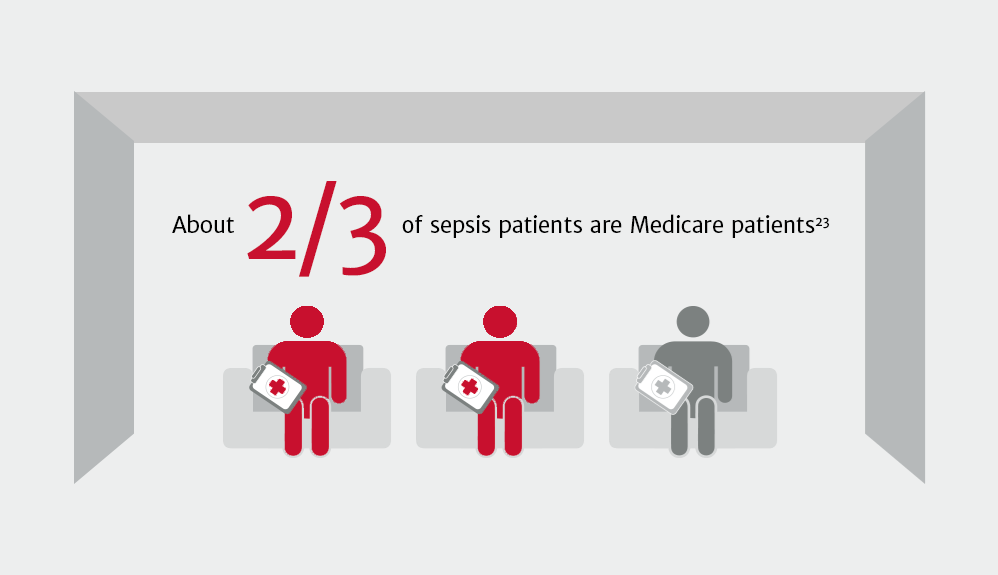
- Statistics, National Center For Health. NCHS Data Brief, Number 62, June 2011 (n.d.): n. pag. www.CDC.gov . Centers for Disease Control, June 2011. Web. 6 Apr. 2016.
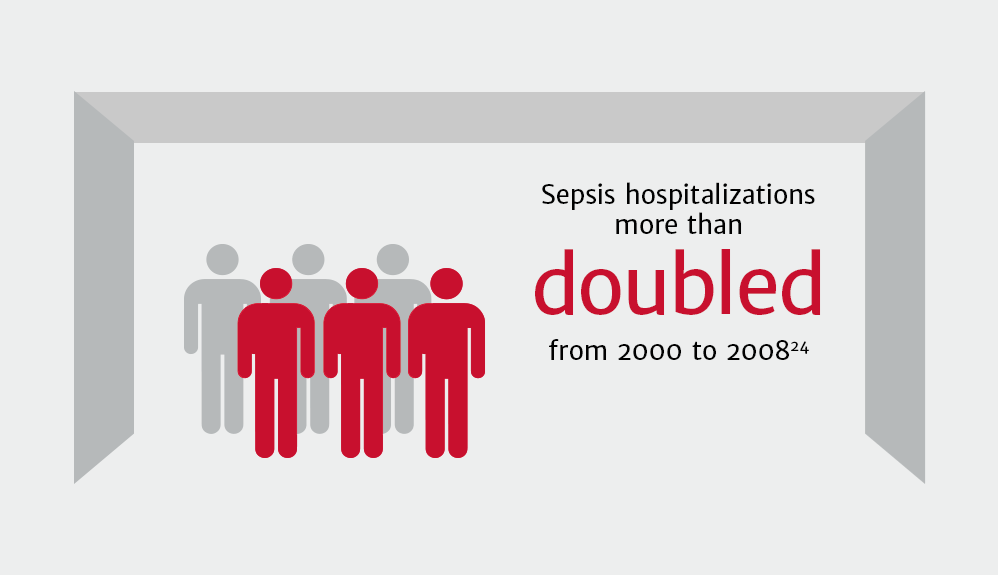
- Statistics, National Center For Health. NCHS Data Brief, Number 62, June 2011 (n.d.): n. pag. www.CDC.gov . Centers for Disease Control, June 2011. Web. 6 Apr. 2016.
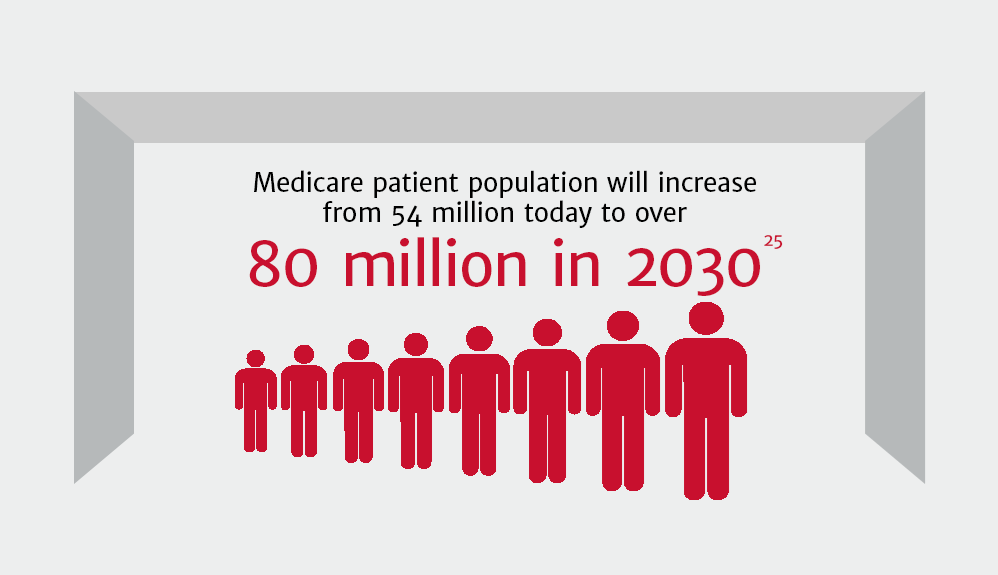
- Report to Congress: Medicare and the Health Care Delivery System, June 2015.
Please update your browser
Please update to a current version of your preferred browser, this site will perform effectively on the following:
Unable to update your browser?If you are on a computer, that is maintained by an admin and you cannot install a new browser, ask your admin about it. If you can't change your browser because of compatibility issues, think about installing a second browser for browsing and keep this old one for compatibility