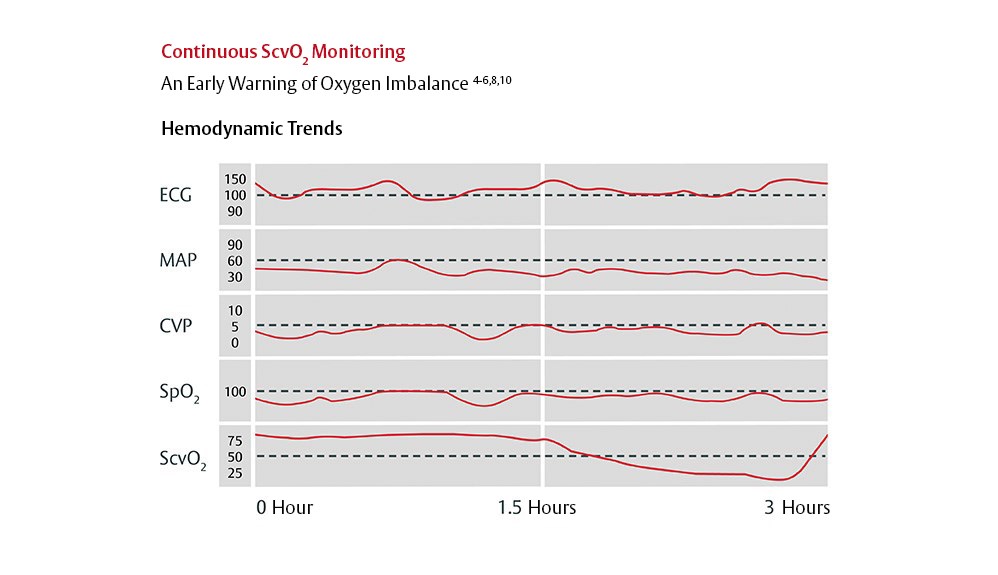
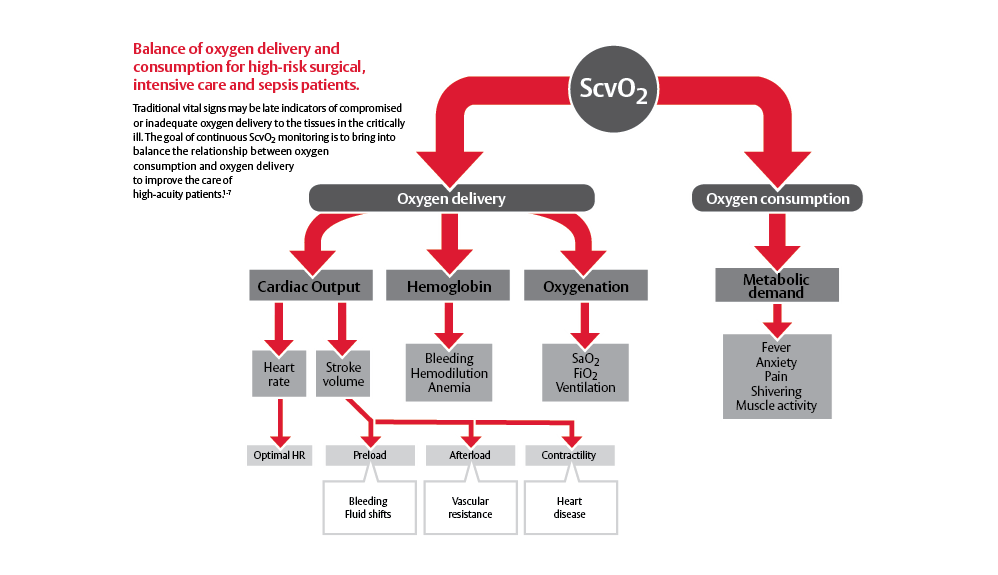
Edwards 中心静脉血氧饱和度导管连续监测中心静脉血氧饱和度(Scv02),这是氧供受损或不足的早期指标。 Edwards 中心静脉血氧饱和度导管通过提供更敏感的氧平衡指标,比传统的生命体征和间断式的采样更早发现关键变化,让您能够更快地辨别和预防组织缺氧。 1-5
参考文献:
- Reinhart K, et al. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30(8):1572-8.
- Rivers EP, et al. Central venous oxygen saturation monitoring in the critically ill patient. Curr Opin Crit Care. 2001;7(3):204-11.
- Ingelmo P, et al. Importance of monitoring in high risk surgical patients. Minerva Anestesiol. 2002;68(4):226-30.
- Scalea, TM, et al. Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma 1990;30(12):1539-43.
- Ander, DS, et al. Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 1998;82(7):888-91.
- Tweddell, JS, et al. Mixed venous oxygen saturation monitoring after stage 1 palliation for hypoplastic left heart syndrome. Ann Thorac Surg 2007;84:1301-1311
- Zaja J. Venous oximetry. Signa Vitae 2007;2(1):6-10.
- Spenceley, N., et al. Continuous central venous saturations during pericardial tamponade case report. Pediatr Crit Care Med 2007,Vol. 8,No. 3,p18.2.153.
- Krahn, G., et al. Early clinical evaluation of the Edwards PediaSat™ oximetry catheter in pediatric patients. Pediatr Crit Care Med 2007,Vol. 8,No. 3,p18.2.152.
- Spenceley, N., et al. Continuous central venous saturation monitoring in pediatrics: a case report. Pediatr Crit Care Med 2008, Vol. 9, No. 2, p e13-e16
- Lemson et al. Advanced hemodynamic monitoring in critically ill patients. Pediatrics. 2011
- GOV FDA 510k EOCVC (K160645)
- EDWARDS OLIGON血气饱和度导管含有集成的OLIGON抗菌材料。 抗菌剂的活性局限于导管表面,不适用于全身性感染的治疗。 体外试验证明,Oligon 材料具有广谱抗菌效果(48小时内由初始浓度下降3个对数单位): 金黄色酿脓葡萄球菌、表皮葡萄球菌、肺炎克雷伯菌、粪肠球菌、白色念珠菌、大肠埃希菌、粘质沙雷氏菌、醋酸钙不动杆菌、白喉杆菌、产气肠杆菌、GMRSa耐甲氧西林金黄色葡萄球菌、铜绿假单胞菌、光滑念珠菌和VRE(屎肠球菌)。
- 美国专利号4411648
- Ranucci M, et al. Impact of oligon central venous catheters on catheter colonization and catheter-related bloodstream infection. Crit Care Med 2003;31(1):52-9.
- Garcia, R, et al. Three years experience in implementing HICPAC recommendations for the reduction of central venous catheter-related bloodstream infections. Poster presentation at National APIC meeting, June 2003.
- Loren D. Continuous venous oximetry in surgical patients. Ann Surg. 1986;203/3:329-333.
- Pearse, R, et al. Changes in central venous saturation after major surgery, and association with outcome. Crit Care 2005;9(6):R694-91.
- Rady, MY, et al. Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med 1996;14(2):218-25.
- Rivers, EP, et al. The clinical implications of continuous central venous oxygen saturation during human CPR. Ann Emerg Med 1992;21(9):1094-101.
- Nakazawa, K, et al. Usefulness of central venous oxygen saturation monitoring during cardiopulmonary resuscitation. A comparative case study with end-tidal carbon dioxide monitoring. Intensive Care Med 1994;20(6):450-1.
- Noguiera P, et al. Central Venous Saturation: A Prognostic Tool in Cardiac Surgery Patients. J Intensive Care Med. 2010;25(2):111-116.
- Vallet B, et al. Venous oxygen saturation as a physiologic transfusion trigger. Crit Care. 2010;14:213.
- Donati A, et al. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk patients. Chest. 2007;132:1817-1824.
- Marik P, et al. Does central venous pressure predict fluid responsiveness? A systemic review of the literature and the Tale of Seven Mares. Chest. 2008;134;172–178
Please update your browser
Please update to a current version of your preferred browser, this site will perform effectively on the following:
Unable to update your browser?If you are on a computer, that is maintained by an admin and you cannot install a new browser, ask your admin about it. If you can't change your browser because of compatibility issues, think about installing a second browser for browsing and keep this old one for compatibility