

血液管理
通过有效的血液管理来保存血液、减少感染并降低输血风险。
血液管理
在OR和ICU的标准操作流程中,将封闭式血液取样(CBS)作为患者血液管理(PBM)流程的一部分可有助于达到积极的患者预后转归,同时可以提供具有成本效益的治疗。与传统血液取样操作相比,已证明CBS可以更有效保存血液、改善患者转归预后并降低成本。12,17,22,23,25
患者血液管理(PBM)及时应用了循证医学和手术概念,旨在通过维持血红蛋白浓度、优化止血并最大限度减少失血来改善患者转归预后。31
常规血液取样操作可能会导致大量失血、不必要的血液浪费和感染风险。临床影响可能包括贫血、输血和医院获得性感染,可导致患者转归不佳不良预后。使用常规血液采集的方法也会使医院成本增加。1-4, 6-9, 11-16, 18, 20-21, 25, 30, 34
封闭式血液取样(CBS)是一种循证解决方案。12,22,23
封闭式血液取样(CBS)是一种循证解决方案。12,22,23
减少失血
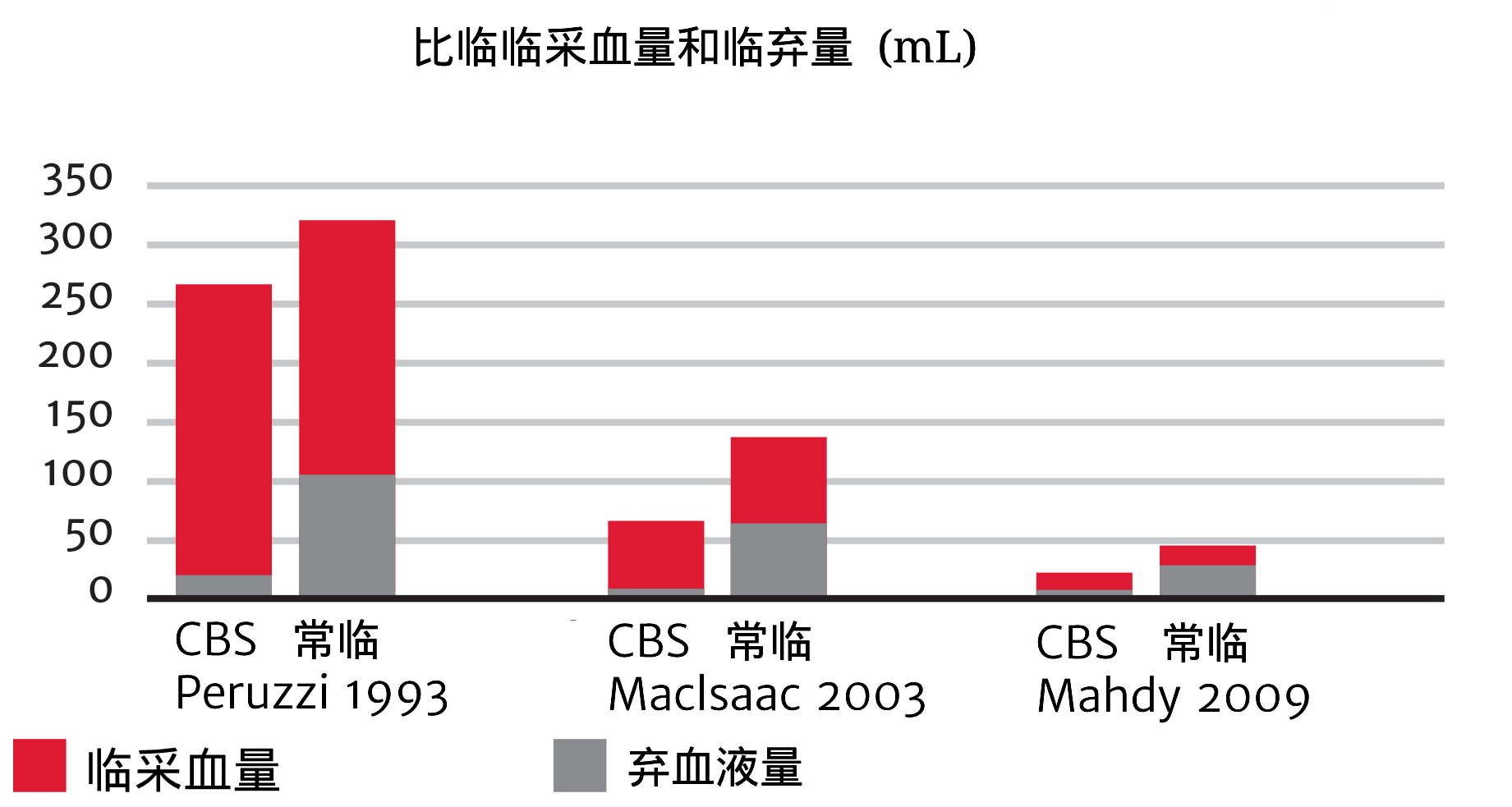
废弃血液占重症患者每日采血总量的
18%至30% 3
- 在ICU,每天采血 5 - 24次1,2
- 每天抽取的血量可能为 26 - 427 mL 2-6
- ICU患者因静脉采血而导致的每周失血量可能为 340 - 660 mL18
- 每次采血废弃的血液为 2 - 10 mL不等3,9
封闭式血液取样(CBS)是一种循证解决方案。12,22,23
减少医源性贫血
取样并废弃导致的失血会导致血红蛋白(Hb)下降,从而引起贫血。13,16-18
.png)
贫血与沉重负担以及器官损伤和死亡的风险增加相关。2,26
减少采血引起的贫血可以减少输血需求。3 此外,通过建立血液管理文化,可以减少医源性贫血。3
- 每采血50 mL,中重度医源性贫血的风险增加18% 3
- 住院时间(LOS)在21天以上的患者,采血量增加超过3.5 mL/天,需要输血以纠正贫血的风险增加2倍 3
- 贫血会对患者的生活质量产生负面影响,并与心脏相关发病率和死亡率的风险增加相关 2,26
封闭式血液取样(CBS)是一种循证解决方案。12,22,23
减少导管相关血流感染(CRBSI)
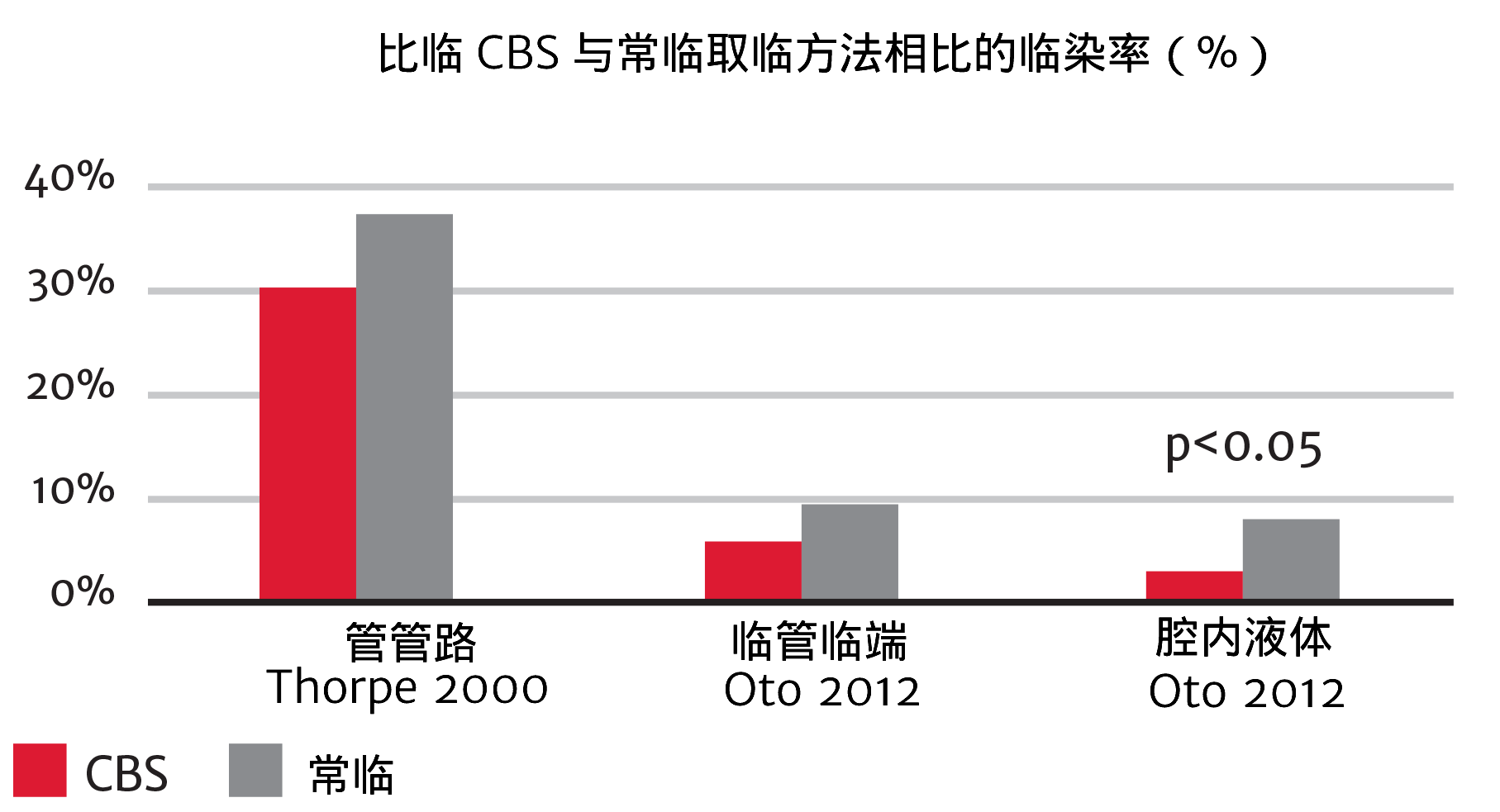
美国每年有50,000名患者发生CRBSI 27
- 在危重病患者中,CRBSI占感染的19%27
- 在儿科ICU,31%的院内感染都是CRBSI27
封闭式血液取样(CBS)是一种循证解决方案。12,22,23
减少输血需求和相关并发症
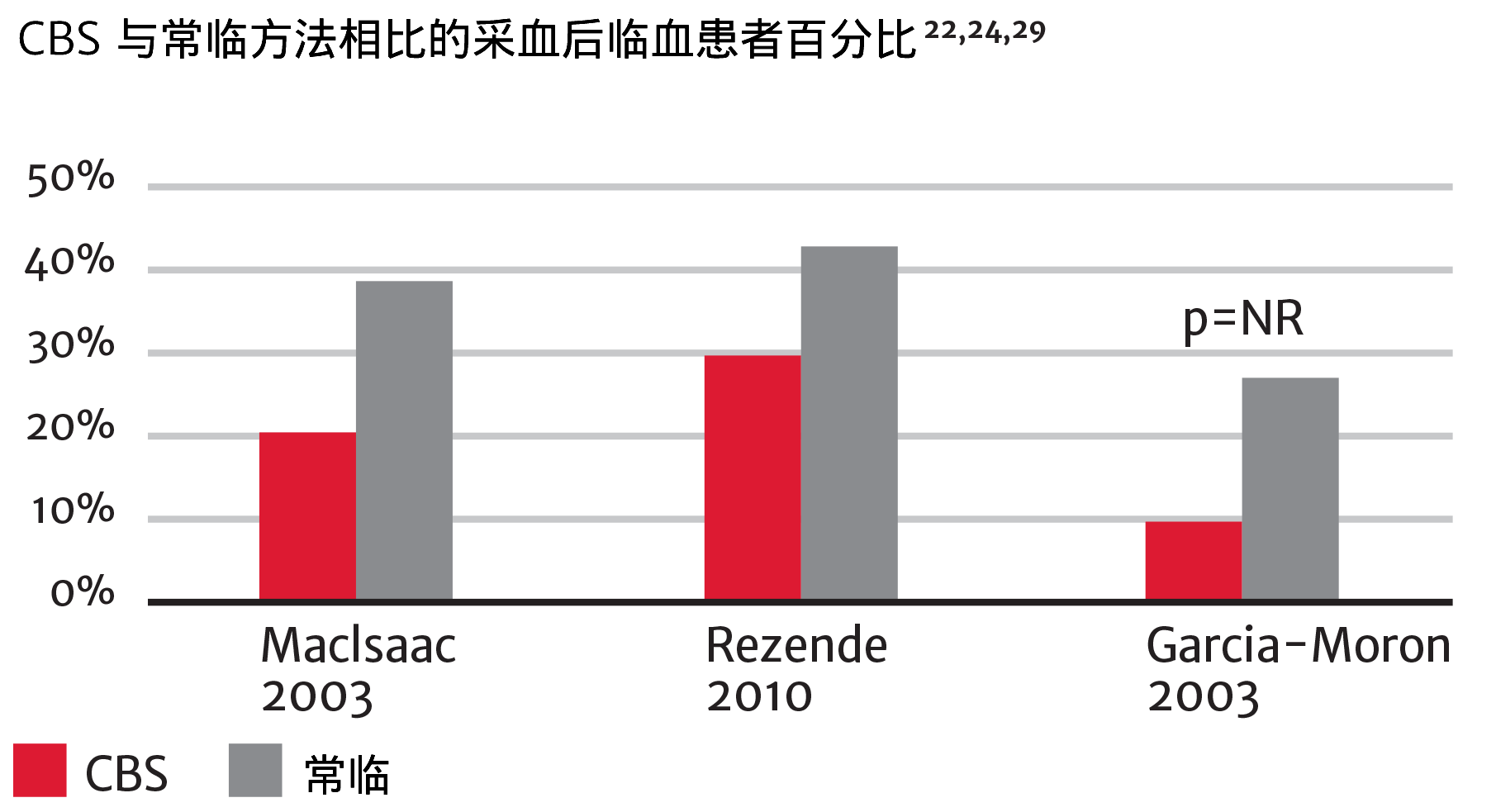
- 输血相关急性肺损伤(TRALI)、输血相关循环超负荷(TACO)、急性呼吸窘迫综合征(ARDS)、感染和呼吸机相关性肺炎 25
- 在各种人群中,红细胞输血与较高的术后感染率相关 2
- 输血患者在ICU和医院的死亡率增加、感染率增加、器官衰竭、ICU住院时间延长24
封闭式血液取样可以通过减少输血发生率来帮助降低医院成本。25
降低住院成本
RBC单位成本为
522 - 118330美元
- 与输血相关的短期和长期不良事件是医疗支出中成本最高的因素之一。33
- 此外,CBS可以通过降低污染风险来帮助您减少因医院获得性并发症(HAC)而造成的处罚。34,35
通过将封闭式血液取样方法纳入患者血液管理项目,可以改善患者预后。32
促进临床进步的血流动力学教育
始终致力于通过教育来改善外科和重症监护患者的护理质量,无论您在学习过程中的哪个阶段,Edwards临床教育都能向您提供一系列的资源和工具,在您目前和未来面临临床挑战时,可以为您不断提供支持。
联系销售代表 联系信息
您的信息已经提交。爱德华生命科学会安排相关人员与您联系。
- Tinmouth, A.T., L.A. McIntyre, and R.A. Fowler, Blood conservation strategies to reduce the need for red blood cell transfusion in critically ill patients. CMAJ :Canadian Medical Association journal = journal de l'Association medicale canadienne, 2008. 178(1):p. 49-57.
- Vincent, J.L., et al., Anemia and blood transfusion in critically ill patients. JAMA, 2002. 288(12): p.1499-507.
- Barth, M.D., et al., Blood Conservation: What Is Current Blood Draw Practice? Journal of infusion nursing : the official publication of the Infusion Nurses Society, 2013. 36(5): p. 323-328.
- Smoller, B.R., M.S. Kruskall, and G.L. Horowitz, Reducing adult phlebotomy blood loss with the use of pediatric-sized blood collection tubes. Am J Clin Pathol, 1989. 91(6): p. 701-3.
- Henry, M.L., W.L. Garner, and P.J. Fabri, Iatrogenic anemia. Am J Surg, 1986. 151(3): p. 362-3.
- Andrews, T., H. Waterman, and V. Hillier, Blood gas analysis: a study of blood loss in intensive care. Journal of advanced nursing, 1999. 30(4): p. 851-7.
- O'Hare, D. and R.J. Chilvers, Arterial blood sampling practices in intensive care units in England and Wales. Anaesthesia, 2001. 56(6): p. 568-71.
- Low, L.L., G.R. Harrington, and D.P. Stoltzfus, The effect of arterial lines on blood-drawing practices and costs in intensive care units. Chest, 1995. 108(1): p. 216-9.
- Yucha, C.B. and E. DeAngelo, The minimum discard volume: accurate analysis of peripheral hematocrit. J Intraven Nurs, 1996. 19(3): p. 141-6.
- Keller, C.A., Methods of drawing blood samples through central venous catheters in pediatric patients undergoing bone marrow transplant: results of a national survey. Oncol Nurs Forum, 1994. 21(5): p. 879-84.
- Holmes, K.R., Comparison of push-pull versus discard method from central venous catheters for blood testing. J Intraven Nurs, 1998. 21(5): p. 282-5.
- Oto, J., et al., Comparison of bacterial contamination of blood conservation system and stopcock system arterial sampling. American Journal of Infection, 2012. 40(6): p. 530-4.
- Thavendiranathan, P., et al., Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. Journal of general internal medicine, 2005. 20(6): p. 520-4.
- Salisbury, A.C., et al., Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Archives of internal medicine, 2011. 171(18): p. 1646-53.
- Chant, C., G. Wilson, and J.O. Friedrich, Anemia, transfusion, and phlebotomy practices in critically ill patients with prolonged ICU length of stay: a cohort study. Critical care, 2006. 10(5): p. R140.
- Lin, J.C., et al., Phlebotomy overdraw in the neonatal intensive care nursery. Pediatrics, 2000. 106(2): p. E19.
- Peruzzi, W.T., et al., A clinical evaluation of a blood conservation device in medical intensive care unit patients. Critical care medicine, 1993. 21(4): p. 501-6.
- Page, C., A. Retter, and D. Wyncoll, Blood conservation devices in critical care: a narrative review. Annals of intensive care, 2013. 3(1): p. 14.
- Corwin, H.L., K.C. Parsonnet, and A. Gettinger, RBC transfusion in the ICU. Is there a reason? Chest, 1995. 108(3): p. 767-71.
- Bateman, S.T., et al., Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med, 2008. 178(1): p. 26-33.
- Corwin, H.L., et al., The CRIT Study: Anemia and blood transfusion in the critically ill—current clinical practice in the United States. Critical care medicine, 2004. 32(1): p. 39-52.
- MacIsaac, C.M., et al., The influence of a blood conserving device on anemia in intensive care patients. Anaesth Intensive Care, 2003. 31(6): p. 653-7.
- Mahdy, S., et al., Evaluation of a blood conservation strategy in the intensive care unit: a prospective, randomised study. Middle East J Anesthesiol, 2009. 20(2): p. 219-23.
- Rezende E, F.M., Manoel Da Silva Junior J, et al, Closed system for blood sampling and transfusion in critically ill patients. Rev Bras Ter Intensiva, 2010. 22: p. 5-10.
- Mukhopadhyay, A., et al., The use of a blood conservation device to reduce red blood cell transfusion requirements: a before and after study. Critical care, 2010. 14(1): p. R7.
- Rudis, M.I., et al., Managing anemia in the critically ill patient. Pharmacotherapy, 2004. 24(2): p. 229-47.
- De Gaudio, A.R. and A. Di Filippo, Device-related infections in critically ill patients. Part I: Prevention of catheter-related bloodstream infections. J Chemother, 2003. 15(5): p. 419-27.
- Crow, S., et al., Microbial contamination of arterial infusions used for hemodynamic monitoring: a randomized trial of contamination with sampling through conventional stopcocks versus a novel closed system. Infection control and hospital epidemiology: the official journal of the Society of Hospital Epidemiologists of America, 1989. 10(12): p. 557-61.
- Moron N., J.E., Moreno I., Lazaro A., Dispositivo VAMP Beneficis para el paciente critico. Rev ROL Enf, 2003. 26(9): p. 591-594.
- Shander, A., et al., Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion, 2010. 50(4): p. 753-65.
- Society for the Advancement of Blood Management, Professional Definition of Patient Blood Management (PBM) on homepage, http://sabm.org, retrieved April 17, 2015.
- Society for the Advancement of Blood Management®. SABM Administrative and Clinical Standards for Patient Blood Management Programs, 3rd Edition. Unpublished work © 2014.
- Shander, A., et al., Estimating the cost of blood: past, present, and future directions. Best Practice & Research Clinical Anaesthesiology, 2007. Vol 21, No. 2, p. 271-289. doi:10.1016/j.bpa.2007.01.002
- Tang, M., et al. Closed Blood Conservation Device for Reducing Catheter-Related Infections in Children After Cardiac Surgery. Crit Care Nurse, 2014. Oct;34(5):53-60. doi:10.4037/ccn2014416.
- CMS.gov Centers for Medicare & Medicaid Services. Hospital-Acquired Condition (HAC) Reduction Program. https://www.qualitynet.org/inpatient/hac
Please update your browser
Please update to a current version of your preferred browser, this site will perform effectively on the following:
Unable to update your browser?If you are on a computer, that is maintained by an admin and you cannot install a new browser, ask your admin about it. If you can't change your browser because of compatibility issues, think about installing a second browser for browsing and keep this old one for compatibility




