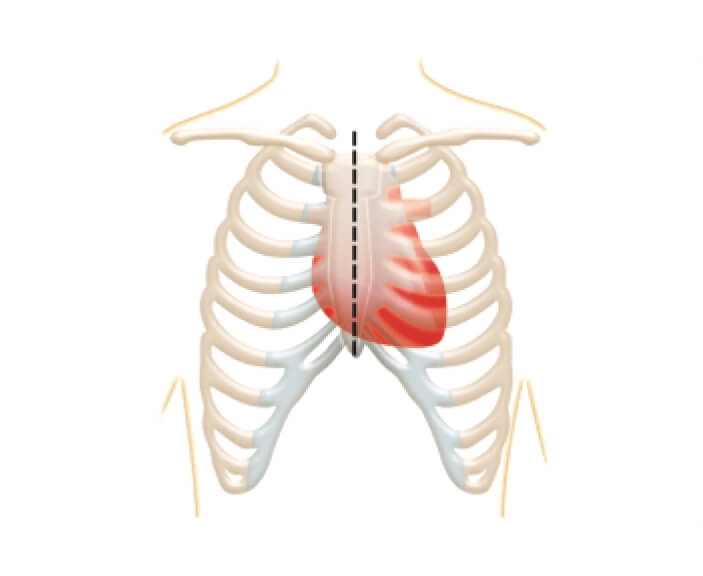
Full sternotomy
Open-heart surgery where the surgeon makes a cut through the breastbone to reach the heart.12

Your doctor may recommend open heart surgery or minimally invasive surgery. Open-heart surgery is accomplished through one incision in the front of your chest. In contrast, minimally invasive surgery is performed through smaller incisions on the side of your chest.1
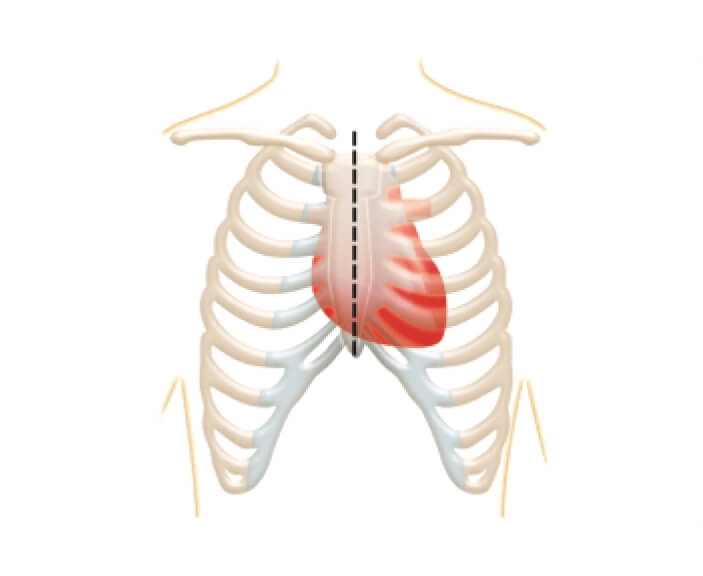
Open-heart surgery where the surgeon makes a cut through the breastbone to reach the heart.12
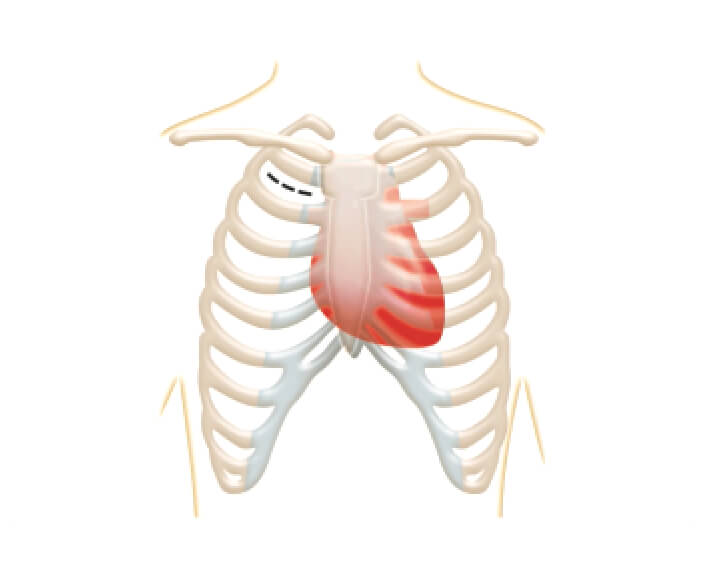
The valve can also be implanted using less invasive methods, such as 'mini thoracotomy,' where a small cut is made between the ribs to access the heart.12 You and your doctor will discuss the best option for you.
Minimally invasive surgery is often associated with less scarring, reduced pain and faster healing.1,2 Minimally invasive surgery still requires a surgical opening and exposes the heart.1 You will need to be put on cardiopulmonary bypass, where a machine temporarily takes over the function of your heart and lungs, for either type of surgery.1 Some surgeons can do both techniques, but some might specialise in one or the other. You and your doctor should discuss the best approach for you.
Even though the idea of heart valve surgery can seem scary, over 6,000 cardiac surgeries are performed in the UK every year.*3 Your doctor will help you make a treatment decision based on your lifestyle and recommended guidelines.4 These recommended guidelines are based on years of heart valve research.
*Based on the average of a 2016–2022 dataset from the UK (excluding Scotland).3
Surgical aortic valve replacement patients need a valve that works for them in the long-term without impacting quality of life. The more durable a valve is, the longer it should last – meaning you have less chance of needing another operation.
You will be fitted with either a tissue or mechanical valve. When choosing a heart valve for your surgical aortic valve replacement, your Heart Team will discuss your options and help you decide what is the best valve replacement choice for you.
Below are some important considerations that may help you with your choice:
| Tissue valves | Mechanical valves | |
| What is the valve made out of? | Animal tissue, such as from cows or pigs5 | Materials such as titanium and carbon5 |
| How long will the valve last? | Approximately 10-20 years*6,7 | Usually lasts a lifetime6 |
| Will I need to be on long-term blood thinning medication? | No4 | Yes, mechanical valves need lifelong use of a blood thinner, which prevents blood clotting4 |
| Do I need to make any lifestyle changes? | No | Yes, taking an anticoagulant means regular monitoring and changing your lifestyle to avoid injuries8 |
| Do I need to consider my diet? | You might need to reduce your calcium intake9 | Keep the amounts of foods high in vitamin K (e.g. leafy greens) consistent in your diet8,10 |
| Will I be able to hear my replacement valve? | No | Yes, you’ll be able to hear some clicking sounds as your valve closes11 |
| What are the risks if I am planning on becoming pregnant in the future? | No known pregnancy complication risk4 | High pregnancy complication risk4 |
*This range is an approximation based on reported outcomes and therefore is not exact. In some circumstances, patients may experience valve deterioration outside of this range.
Unlike tissue valves, people with mechanical valves need to take a particular type of blood thinner known as a vitamin K antagonist for the rest of their lives.4 This is an important consideration, especially if you can’t take blood thinners because of a history of bleeding or you have an increased risk of injury or bleeding because of work, lifestyle or sports.
Patients on a vitamin K antagonist must:8