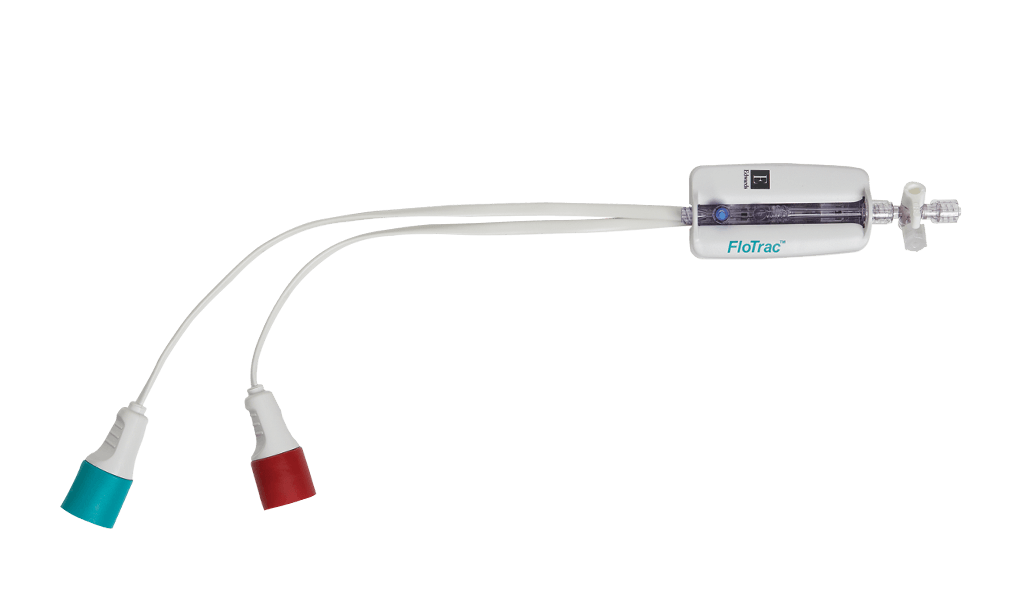
PediaSat oximetry catheter
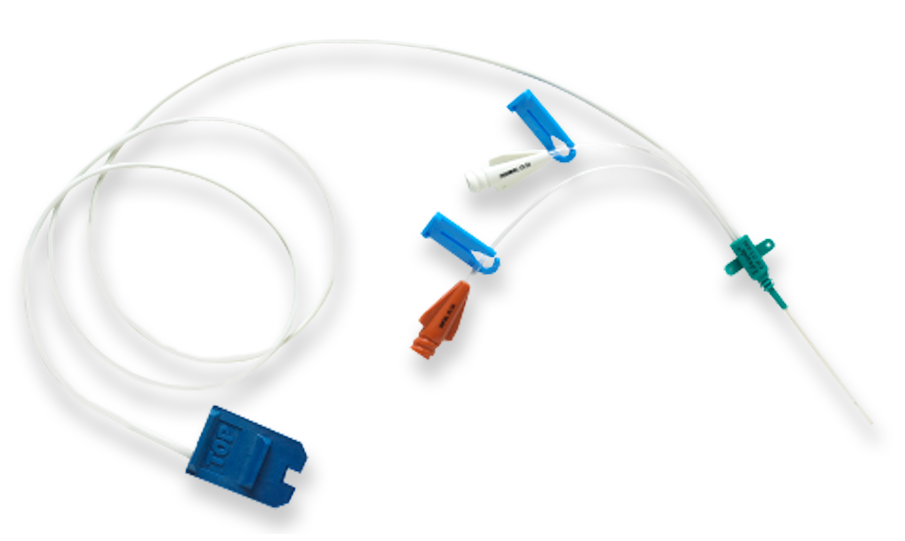
PediaSat oximetry catheter is the first and only pediatric oximetry catheter with continuous ScvO2 monitoring for proactive management of tissue hypoxia.1-3 Continuous, real-time monitoring of central venous oxygen saturation (ScvO2) offers early recognition of critical changes in oxygen delivery that may not be identified by less sensitive indicators, such as traditional vital signs or intermittent sampling.2-8
PediaSat oximetry catheter
Continuous ScvO2 monitoring

Early warning of oxygen imbalance allows early intervention.2,4,6,9-11
Early indication with continuous ScvO2 monitoring offers you the ability to detect and prevent tissue hypoxia − early− in your complex pediatric patients.2,6,9-11
Continuous ScvO2 monitoring reveals the root cause of oxygen imbalance, enabling you to proactively determine appropriate therapy.2,4,5,7,12 Real-time insight into the adequacy of cardiac output allows immediate assessment of your patient's clinical response to therapy − to help you stay ahead of tissue hypoxia and stages of sepsis.
Continuous ScvO2 monitoring helps guide therapy and enables early intervention:2,4,7
You can use hemodynamics to manage pediatric and neonatal septic shock patients in accordance with ACCM-PALS Clinical Practice Parameters13
PediaSat oximetry catheter model numbers
For more information, please contact your local sales representative.
Customer_Service_ca@Edwards.com
Philips IntelliVue SO2 module
| M1011A* | SO2 Module |
| 989803151591* | Optical Module |
*Philips Healthcare model numbers
Clinical application
See clearly. Stay ahead.
PediaSat oximetry catheter offers an early warning for compromised or inadequate oxygen delivery2,4,6,9-11
Continuous measurement of ScvO2 in combination with other surrogates of organ perfusion (vital signs, lactate, etc.) can be used as a reliable monitor of cardiocirculatory function.3
- Detect acute changes in systemic oxygen delivery and consumption14
- Identify decreases in systemic oxygen delivery that otherwise would not be identified using intermittent sampling8
- Evaluate oxygen reserve to decide routine interventions (including suctioning, turning, etc.) to minimize patient compromise and maximize outcome.15
Can optimize hemodynamic management in complex pediatric patients.1,11,15-17
- Congenital heart disease and other complex cardiac patients1,16
- Sepsis and septic shock17
- Acute respiratory distress syndrome (ARDS)15
- Other high-risk patients11
Convenient, accurate and easy to use.3,12,18
PediaSat oximetry catheter provides:
- Simplicity and flexibility − uses the same insertion techniques as central lines in typical pediatric insertion sites, including subclavian and internal jugular
- Continuous ScvO2 monitoring, pressure monitoring and infusion of solutions
- Accurate oxygenation status1,2
- Double and triple lumens to monitor and administer solutions
References
- Ranucci, M., et al. Continuous monitoring of Central venous oxygen saturation (PediaSat) in pediatric patients undergoing cardiac surgery: a validation study of a new technology. Journal of cardiothoracic and vascular anesthesia, Vol. 22, No. 6, December 2008, p. 847-852.
- Reinhart K, et al. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30(8):1572-8.
- Mahajan A, et al. An experimental and clinical evaluation of a novel central venous catheter with integrated oximetry for pediatric patients undergoing cardiac surgery. Pediatric Central Venous Oximetry. Anest Anal. 2007;Vol.105, No. 6, 1598.
- Rivers EP, et al. Central venous oxygen saturation monitoring in the critically ill patient. Curr Opin Crit Care. 2001;7(3):204-11.
- Pearse, R, et al. Changes in central venous saturation after major surgery, and association with outcome. Crit Care 2005;9(6):R694-91.
- Scalea, TM, et al. Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma 1990;30(12):1539-43.
- Tweddell, JS, et al. Mixed venous oxygen saturation monitoring after stage 1 palliation for hypoplastic left heart syndrome. Ann Thorac Surg 2007;84:1301-1311.
- Tweddell JS, et al. Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg. 2000;69(6):1893-9.
- Ingelmo P, et al. Importance of monitoring in high-risk surgical patients. Minerva Anestesiol. 2002;68(4):226-30.
- Ander, DS, et al. Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 1998;82(7):888-91.
- Ranucci et al. Central venous oxygen saturation and blood lactate levels during cardiopulmonary bypass are associated with outcome after pediatric cardiac surgery. Critical Care 2010.
- Vallet B, et al. Venous oxygen saturation as a physiologic transfusion trigger. Crit Care. 2010;14:213.
- de Oliveira, CF, et al. An outcomes comparison of ACCM/PALS guidelines for pediatric septic shock with and without central venous oxygen saturation monitoring. Pediatr Crit Care Med 2007, Vol. 8,No. 3 (Suppl.).
- Tweddell JS, et al. Postoperative management in patients with complex congenital heart disease. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2002;5:187-205.
- Sanders CL. Making clinical decisions using SvO2 in PICU patients. Dimens Crit Care Nurs. 1997;16(5):257-64.
- Mohseni, H, et al. Evaluation of a new pediatric continuous oximetry catheter. Pediatr Crit Care Med 2011;12(4): 437-441.
- Lemson et al. Advanced hemodynamic monitoring in critically ill patients. Pediatrics. 2011.
- Ranucci, M, et al. Near-infrared spectroscopy correlates with continuous superior vena cava oxygen saturation in pediatric cardiac surgery patients. Pediatric Anesthesia 2008. 18:1163-1169.