How you manage volume matters
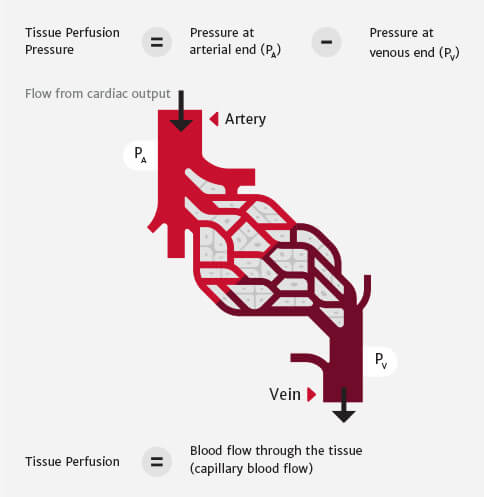
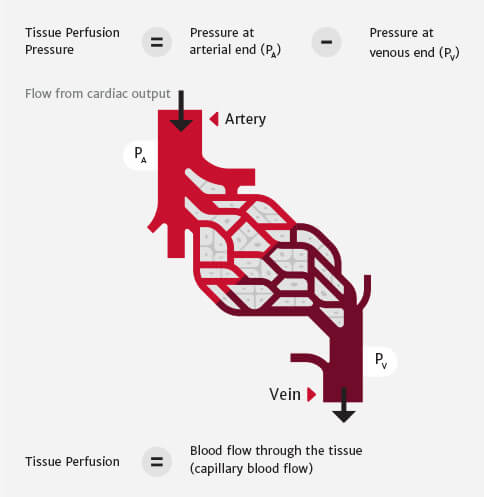
Physiology of perfusion: pressure and flow
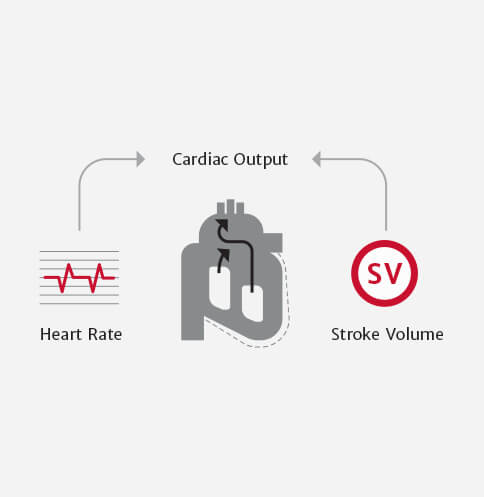
Cardiac Output (CO) = Stroke Volume x Heart Rate
Managing the flow component of perfusion
Maintaining patients in the optimal volume range is key. Using dynamic and flow-based parameters to guide fluid administration helps maintain patients in the optimal volume range.1
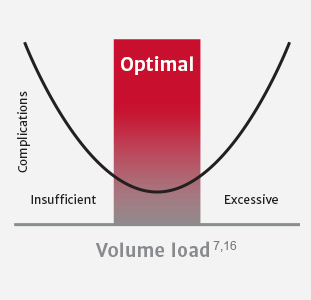
Insufficient volume administration is associated with:
- GI dysfunction (postoperative ileus, PONV, upper GI bleeding, anastomotic leak)2
- Infectious complication (tissue hypoperfusion)2,3
- Acute renal insufficiency or failure4
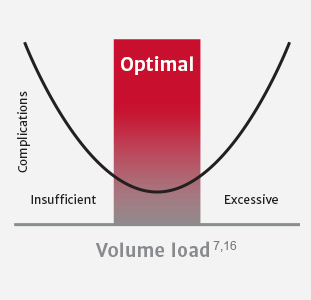
Excessive volume administration is associated with:
- Pulmonary edema5
- GI dysfunction (abdominal compartment syndrome, ileus, anastomotic leak)17,18,19
- Coagulopathy5
Individualizing volume management
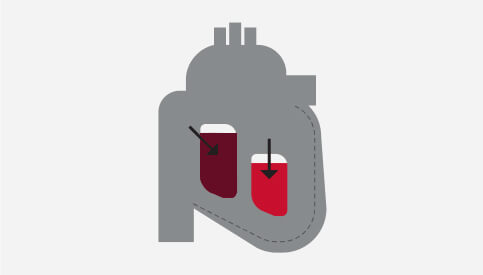
Preload: the tension of myocardial fibers at the end of diastole, as a result of volume in the ventricle
Stroke Volume (SV): volume of blood pumped from the left ventricle per heartbeat
When managing perfusion, stroke volume can be optimized using the patient’s own Frank-Starling curve — a plot of stroke volume (SV) vs. preload.
Stroke volume is optimized when it resides at the shoulder of the Frank-Starling curve (refer to figure below).
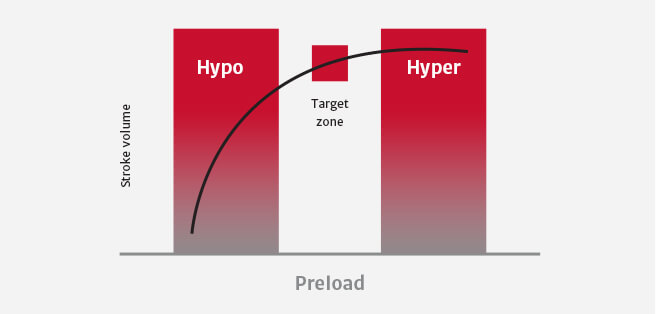
The patient’s location on his or her Frank-Starling curve can be determined by measuring ∆SV in response to change in preload using:
Fluid bolus challenge
Passive leg raise (PLR)
Dynamic and flow-based parameters are more informative than conventional parameters in determining fluid responsiveness and may help you avoid excessive and insufficient fluid administration.7
Clinical studies have shown that conventional volume management methods, based on conventional parameters, are misleading and insensitive.6
Advanced hemodynamic parameters such as stroke volume (SV) and stroke volume variation (SVV), are key to optimal fluid administration.6
SVV has been proven to be a highly sensitive and specific indicator for preload responsiveness when managing perfusion. As a dynamic parameter, SVV has been shown to be an accurate predictor of fluid responsiveness in loading conditions induced by mechanical ventilation.6,8,20
Research demonstrating the value of dynamic and flow-based parameters
- Thacker, et al. Perioperative Fluid Utilization Variability and Association With Outcomes: Considerations for Enhanced Recovery Efforts in Sample US Surgical Population. Ann Surg 2015
- Peng, K., et al., Goal-directed fluid therapy based on stroke volume variations improves fluid management and gastrointestinal perfusion in patients undergoing major orthopedic surgery. Med Princ Pract, 2014
- Dalfino et al. Haemodynamic goal-directed therapy and postoperative infections: earlier is better. A systematic review and meta-analysis. Crit Care 2011
- Giglio, MT et al. Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials. British Journal of Anesthesia 2009
- Shin, C. et al. Effects of Intraoperative Fluid Management on Postoperative Outcomes: A Hospital Registry Study. Annals of Surgery 2017
- Sun, Y. et al. Effect of perioperative goal-directed hemodynamic therapy on postoperative recovery following major abdominal surgery-a systematic review and meta-analysis of randomized controlled trials. Critical Care 2017
- Goepfert, M.S., et al., Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology, 2013
To learn more about managing fluid with advanced parameters, contact us today.
Reducing variability using perioperative goal-directed therapy (PGDT)
Post-surgical complications have an impact on human life.9

Major complications occur in approximately 16% of surgeries.9
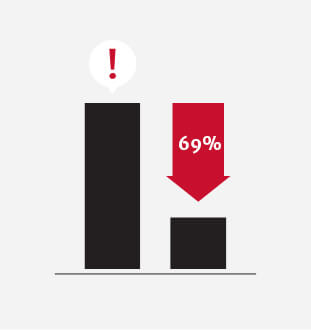
Independent of preoperative patient risk, the occurrence of even a single post-surgical complication within 30 days reduced median patient survival by 69%.10

Hemodynamic optimization through PGDT is demonstrated to reduce complications like acute kidney injury (AKI) and surgical site infection (SSI), as well as reduce length of stay, and associated costs in your moderate- to high-risk surgery patients.11,12
Hemodynamic optimization through PGDT may:
Reduce post-surgical complications by an average of 32%13

Reduce average hospital length of stay: 1+ days13,14

Approximate extra cost of treating one post-operative complication: $18,0000-$20,00015
PGDT is a treatment protocol using dynamic and flow-based hemodynamic parameters with the objective of making the appropriate volume management decisions. PGDT can be implemented in a single procedure or as part of a larger initiative such as Enhanced Recovery After Surgery pathways.
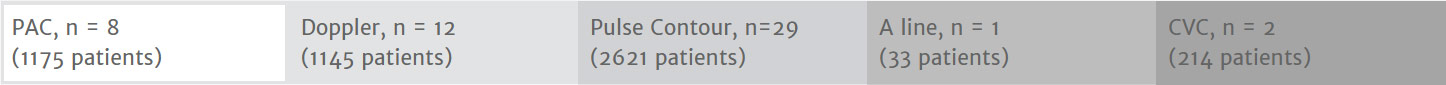
50+ studies demonstrating the use of PGDT
50+ randomized controlled trials and 14+ meta-analyses have demonstrated clinical benefits of hemodynamic optimization over standard volume management.
Studies
- Michard, et al. Perioperative goal-directed therapy with uncalibrated pulse contour methods: impact on fluid management and postoperative outcome. British Journal of Anesthesia 2017
- Pearse, R. et al. Effect of a Perioperative, Cardiac Output–Guided Hemodynamic Therapy Algorithm on Outcomes Following Major Gastrointestinal Surgery A Randomized Clinical Trial and Systematic Review. JAMA 2014
- Grocott, MP et al. Perioperative increase in global blood flow to explicit defined goals and outcomes after surgery: a Cochrane Systematic Review. British Journal of Anesthesia 2013
- Thiele et al. American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on perioperative fluid management within an enhanced recovery pathway for colorectal surgery. Periop Med 2016
- Ramsingh , et al. Outcome impact of goal directed fluid therapy during high risk abdominal surgery in low to moderate risk patients: a randomized controlled trial. J Clin Monit Comput 2011
- Cecconi, et al. Goal directed haemodynamic therapy during elective total hip arthroplasty under regional anaesthesia. Crit Care 2011
View the complete list of studies
Randomized Controlled Trials Showing a Benefit in Perioperative Goal-Directed Therapy
More than 3000 patients have been enrolled in these 52 positive RCTs.
| Title, author and year | n | Parameters optimized | Surgery | Tool | Main benefits |
| Prospective trial of supranormal values of survivors as therapeutic goals in high-risk patients. Shoemaker 1988 | 310 | DO2 | General | PAC-1 | Morbidity Mortality (21 vs 34%) Cost-savings |
| Preoperative optimization of cardiovascular hemodynamics improves outcomes in peripheral vascular surgery. Berlauk 1991 | 89 | CI, PCWP, SVR | Vascular | PAC-2 | Morbidity |
| Prospective trial of supranormal values as goals of resuscitation in severe trauma. Fleming 1992 | 67 | DO2 | Trauma | PAC-3 | Morbidity |
| A randomized clinical trial of the effect of deliberate perioperative increase of oxygen delivery on mortality in high-risk patients. Boyd 1993 | 107 | DO2 | General | PAC-4 | Morbidity Mortality (6 vs 22%) Cost-savings |
| Perioperative plasma volume expansion reduces the incidence of gut mucosal hypoperfusion during cardiac surgery. Mythen 1995 | 60 | SV | Cardiac | Doppler-1 | Morbidity Hospital LOS |
| Intraoperative intravascular volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. Sinclair 1997 | 40 | SV | Hip | Doppler-2 | Hospital LOS |
| Response of patients with cirrhosis who have undergone partial hepatectomy to treatment aimed at achieving supranormal oxygen delivery and consumption. Ueno 1998 | 34 | DO2 | Hepatectomy | PAC-5 | Morbidity |
| Reducing the risk of major elective surgery: randomised controlled trial of preoperative optimization of oxygen delivery. Wilson 1999 | 138 | DO2 | General and vascular | PAC-6 | Morbidity Hospital LOS Cost-savings |
| A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Polonen 2000 | 393 | SvO2 | Cardiac | PAC-7 | Morbidity Hospital LOS |
| Effects of maximizing oxygen delivery on morbidity and mortality in high-risk surgical patients. Lobo 2000 | 37 | DO2 | General | PAC-8 | Morbidity Mortality (16 vs 50%) |
| Randomized controlled trial to investigate influence of the fluid challenge on duration of hospital stay and perioperative morbidity in patients with hip fractures. Venn 2002 | 59 | SV | Hip | Doppler-3 | Morbidity |
| Goal-directed Intraoperative fluid administration reduces length of hospital stay after major surgery. Gan 2002 | 100 | SV | General | Doppler-4 | Morbidity Hospital LOS |
| Randomised controlled trial investigating the influence of intravenous fluid titration using oesophageal Doppler monitoring during bowel surgery. Conway 2002 | 57 | SV | Bowel | Doppler-5 | Morbidity |
| Randomised controlled trial assessing the impact of a nurse delivered, flow monitored protocol for optimisation of circulatory status after cardiac surgery. McKendry 2004 | 174 | SV | Cardiac | Doppler-6 | Hospital LOS |
| Intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Wakeling 2005 | 128 | SV | Bowel | Doppler-7 | Morbidity Hospital LOS |
| Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial. Pearse 2005 | 122 | DO2 | General | LidCO-1 | Morbidity Hospital LOS |
| Randomized clinical trial assessing the effect of Doppler- optimized fluid management on outcome after elective colorectal resection. Noblett 2006 | 108 | SV | Bowel | Doppler-8 | Morbidity Hospital LOS |
| Esophageal Doppler-guided fluid management decreases blood lactate levels in multiple-trauma patients: a randomized controlled trial. Chytra 2007 | 162 | SV | Trauma | Doppler-9 | Morbidity Hospital LOS |
| Goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery: a pilot randomized controlled trial. Lopes 2007 | 33 | PPV | General | A line-1 | Morbidity Hospital LOS |
| Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Donati 2007 | 135 | ERO2 | General and vascular | CVC-1 | Morbidity Hospital LOS |
| Goal-directed intraoperative therapy based on Autocalibrated arterial pressure waveform analysis reduces hospital stay in high-risk surgical patients: a randomized, controlled trial. Mayer 2009 | 60 | SVV, SVI, CI | Abdominal | FloTrac sensor-1 | Morbidity Hospital LOS |
| Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Benes 2010 | 120 | SVV, CI | Abdominal and vascular | FloTrac sensor-2 | Morbidity |
| Haemodynamic optimisation improves tissue microvascular flow and oxygenation after major surgery: a randomised controlled trial. Jhanji 2010 | 135 | SV, DO2 | Abdominal | LidCO-2 | Morbidity |
| Goal-directed haemodynamic therapy during elective total hip arthroplasty under regional anaesthesia. Cecconi 2011 | 40 | DO2 | Hip | FloTrac sensor-3 | Morbidity |
| A double-blind randomized controlled clinical trial to assess the effect of doppler optimized intraoperative fluid management on outcome following radical cystectomy. Pillai 2011 | 66 | SV | Cyctectomy | Doppler-10 | Morbidity |
| Haemodynamic optimisation in lower limb arterial surgery: room for improvement? Bisgaard 2012 | 40 | SV, DO2 | Vascular | LidCO-3 | Morbidity |
| Outcome impact of goal directed fluid therapy during high risk abdominal surgery in low to moderate risk patients: a randomized controlled trial. Ramsingh 2012 | 38 | SVV | Abdominal | FloTrac sensor-4 | Morbidity Hospital LOS |
| Goal-directed intraoperative fluid therapy guided by stroke volume and its variation in high-risk surgical patients: a prospective randomized multicentre study. Scheeren 2012 | 40 | SVV, SV | Abdominal | FloTrac sensor-5 | Morbidity |
| Intraoperative fluid management in open gastrointestinal surgery: goal-directed versus restrictive. Zhang 2013 | 80 | SVV, CI | Thoracic | FloTrac sensor-6 | Morbidity |
| Individually optimized hemodynamic therapy reduces complications and length of stay in the Intensive Care Unit. Goepfert 2013 | 100 | SVV, GEDI, CI, EVLW | Cardiac | PiCCO-1 | Morbidity |
| Perioperative goal-directed hemodynamic therapy based on radial arterial pulse pressure variation and continuous cardiac index trending reduces postoperative complications after major abdominal surgery: a multi-center, prospective, randomized study. Salzwedel 2013 | 160 | PPV, CI | Abdominal | ProAQT-1 | Morbidity Hospital LOS |
| Goal-directed fluid therapy in gastrointestinal surgery in older coronary heart disease patients: randomized trial. Zheng 2013 | 60 | SVV, SVI, CI | Abdominal | FloTrac sensor-7 | Morbidity Hospital LOS |
| Zakhaleva, J., et al., The impact of intravenous fluid administration on complication rates in bowel surgery within an enhanced recovery protocol: a randomized controlled trial. Colorectal Dis, 2013. 15(7): p. 892-9 | 91 | SV | Abdominal surgery | TED | Morbidity |
| Peng, K., et al., Goal-directed fluid therapy based on stroke volume variations improves fluid management and gastrointestinal perfusion in patients undergoing major orthopedic surgery. Med Princ Pract, 2014. 23(5): p. 413-20 | 80 | SVV | Orthopedic surgery | PC FloTrac sensor | GI recovery |
| Zeng, K., et al., The influence of goal-directed fluid therapy on the prognosis of elderly patients with hypertension and gastric cancer surgery. Drug Des Devel Ther, 2014. 8: p. 2113-9 | 60 | SVV | Gastrectomy | PC FloTrac sensor | Morbidity, hospital length of stay |
| Colantonio, L., et al., A randomized trial of goal directed vs. standard fluid therapy in cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. J Gastrointest Surg, 2015. 19(4): p. 722-9 | 80 | CI, SVI | Cytoreductive surgery | PC FloTrac sensor | Morbidity, hospital length of stay |
| Funk, D.J., et al., A randomized controlled trial on the effects of goal-directed therapy on the inflammatory response open abdominal aortic aneurysm repair. Crit Care, 2015. 19: p. 247 | 40 | SVV, CI | Vascular surgery | PC FloTrac sensor | Morbidity |
| Mikor, A., et al., Continuous central venous oxygen saturation assisted intraoperative hemodynamic management during major abdominal surgery: a randomized, controlled trial. BMC Anesthesiol, 2015. 15: p. 82 | 79 | ScvO2 | Abdominal surgery | CVC Cevox | Mortality and oxygen delivery |
| Han, G., et al., Application of LiDCO-Rapid in peri-operative fluid therapy for aged patients undergoing total hip replacement. International Journal of Clinical and Experimental Medicine, 2016. 9(2): p. 4473-4478 | 40 | SVV | Orthopedic surgery | PC LiDCO rapid | Morbidity |
| Hand, W.R., et al., Intraoperative goal-directed hemodynamic management in free tissue transfer for head and neck cancer. Head Neck, 2016. 38 Suppl 1: p. E1974-80 | 94 | SVV, CI, SVR | Free tissue surgery | PC FloTrac sensor | ICU length of stay |
| Kapoor, P.M., et al., Perioperative utility of goal-directed therapy in high-risk cardiac patients undergoing coronary artery bypass grafting: “A clinical outcome and biomarker- based study”. Ann Card Anaesth, 2016. 19(4): p. 638-682 | 130 | SVV, CI, SVI, SVRI, DO2 | Cardiac surgery | PC FloTrac sensor, Edwards oximetry CVC | ICU Length of Stay, Hospital Length of Stay |
| Kumar, L., S. Rajan, and R. Baalachandran, Outcomes associated with stroke volume variation versus central venous pressure guided fluid replacements during major abdominal surgery. J Anaesthesiol Clin Pharmacol, 2016. 32(2): p. 182-6 | 60 | SVV | Abdominal surgery | PC FloTrac sensor | ICU Length of Stay |
| Osawa, E.A., et al., Effect of Perioperative Goal-Directed Hemodynamic Resuscitation Therapy on Outcomes Following Cardiac Surgery: A Randomized Clinical Trial and Systematic Review. Crit Care Med, 2016. 44(4): p. 724-33 | 126 | CI, SVI | Cardiac surgery | PC LidCO Rapid | Morbidity, ICU Length of Stay, Hospital Length of Stay |
| Yuanbo, Z., et al., ICU management based on PiCCO parameters reduces duration of mechanical ventilation and ICU length of stay in patients with severe thoracic trauma and acute respiratory distress syndrome. Annals of Intensive Care, 2016. 6(1): p. 113 | 264 | ITBVI, EVLWI, CI | ICU treatment of ARDS | PC PiCCO | MV days, ICU Length of stay and Cost savings |
| Elgendy, M.A., I.M. Esmat, and D.Y. Kassim, Outcome of intraoperative goal-directed therapy using Vigileo/FloTrac in high-risk patients scheduled for major abdominal surgeries: A prospective randomized trial. Egyptian Journal of Anaesthesia, 2017 | 86 | SVV, CI, MAP | Major abdominal surgery | PC FloTrac sensor | Morbidity, ICU length of stay |
| Kapoor, P.M., et al., Goal-directed therapy improves the outcome of high-risk cardiac patients undergoing off-pump coronary artery bypass. Ann Card Anaesth, 2017. 20(1): p. 83-89 | 163 | SVV, CI, ScvO2 | Cardiac surgery | VolumeView set, PC FloTrac sensor | ICU Length of Stay, Hospital Length of Stay |
| Kaufmann, K.B., et al., Oesophageal Doppler guided goal-directed haemodynamic therapy in thoracic surgery - a single centre randomized parallel-arm trial. Br J Anaesth, 2017. 118(6): p. 852-861 | 100 | SV, CI MAP | Thoracic surgery | TED | Morbidity, Hospital Length of Stay |
| Liang, M., et al., Effect of goal-directed fluid therapy on the prognosis of elderly patients with hypertension receiving plasmakinetic energy transurethral resection of prostate. Int J Clin Exp Med, 2017. 10(1): p. 1290-1296 | 60 | SVV | Urological- Prostate resection | PC FloTrac sensor | Morbidity, Hospital Length of Stay |
| Luo, J., et al., Goal-directed fluid restriction during brain surgery: a prospective randomized controlled trial. Ann Intensive Care, 2017. 7(1): p. 16 | 145 | SVV, CI | Neuro- surgery | PC FloTrac sensor | ICU length of stay and costs, morbidity |
| Weinberg, L., et al., Restrictive intraoperative fluid optimisation algorithm improves outcomes in patients undergoing pancreaticoduodenectomy: A prospective multicentre randomized controlled trial. PLoS One, 2017. 12(9): p. e0183313 | 52 | SVV, CI | Abdominal | PC FloTrac sensor | Morbidity, Hospital Length of Stay |
| Wu, C.Y., et al., Comparison of two stroke volume variation-based goal-directed fluid therapies for supratentorial brain tumour resection: a randomized controlled trial. Br J Anaesth, 2017. 119(5): p. 934-942 | 80 | SVV | Neuro- surgery | PC FloTrac sensor | ICU length of stay, morbidity |
| Wu, J., et al., Goal-directed fluid management based on the auto-calibrated arterial pressure-derived stroke volume variation in patients undergoing supratentorial neoplasms surgery. INTERNATIONAL JOURNAL OF CLINICAL AND EXPERIMENTAL MEDICINE, 2017. 10(2): p. 3106-3114 | 66 | SVV, CI, MAP | Brain surgery | PC FloTrac sensor | Morbidity lactate |
References
- Benes, J., Giglio M., Michard, F. (2014) The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Critical Care, 18(5), 584
- Giglio, MT., Marucci, M., Testini, M., Brienza, N. (2009) Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials. British Journal of Anaesthesia, 103(5), 637-46
- Johnson, A., Ahrens, T. (2015) Stroke Volume Optimization: The New Hemodynamic Algorithm. Critical Care Nurse, 35(1), 11-27
- O’Leary, M. (2001) Preventing renal failure in the critically ill. BMJ, 322(7300), 1437-1439
- Holte, K. (2010) Pathophysiology and clinical implications of perioperative fluid management in elective surgery. Danish Medical Bulletin, 57(7), B4156
- Berkenstadt, H., et al. (2001) Stroke Volume Variation as a Predictor of Fluid Responsiveness in Patients Undergoing Brain Surgery. Anesthesia & Analgesia, 92, 984-9
- Cannesson, M. (2010) Arterial pressure variation and goal-directed fluid therapy. Journal of Cardiothoracic and Vascular Anesthesia, 24(3), 487-97
- Peng, K., Li, J., Cheng, H., Ji, FH. (2014) Goal-directed fluid therapy based on stroke volume variations improves fluid management and gastrointestinal perfusion in patients undergoing major orthopedic surgery. Medical Principles and Practice, 23(5), 413-20
- Ghaferi, A., Birkmeyer, J., Dimick, J. (2009) Variation in hospital mortality associated with inpatient surgery. New England Journal of Medicine, 361(14), 1368-75
- Khuri, S., Henderson, W., DePalma, R., Mosca, C., Healey, N., Kumbhani, D. (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Annals of Surgery, 242(3), 326-41
- Aya, H., Cecconi, M., Hamilton, M., Rhodes, A. (2013) Goal-directed therapy in cardiac surgery: a systematic review and meta-analysis. British Journal of Anaesthesia, 110(4), 510-7
- Brienza, N., Giglio, M., Marucci, M., Fiore, T. (2009) Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study. Critical Care Medicine, 37(6), 2079-90
- Grocott, M., Dushianthan, A., Hamilton, M., Mythen, M., Harrison, D., Rowan, K. (2012) Perioperative increase in global blood flow to explicit defined goals and outcomes following surgery. Cochrane Database of Systematic Reviews, 11, CD004082
- Corcoran, T., Rhodes, J., Clarke, S., Myles, P., Ho, K. (2012) Perioperative fluid management strategies in major surgery: a stratified meta-analysis. Anesthesia & Analgesia, 114(3), 640-51
- Boltz, M., Hollenbeak, C., Ortenzi, G., Dillon, P. (2012) Synergistic implications of multiple postoperative outcomes. American Journal of Medical Quality, 27(5), 383-90
- Bellamy, M. (2006) Wet, dry or something else? British Journal of Anaesthesia, 97(6), 755-7
- Ping W, et al. Effects of Stroke Volume Variability-Guided Intraoperative Fluid Restriction on Gastrointestinal Functional Recovery. Chinese Journal of Anesthesiology 31.1 (2011): 78-81.
- Thacker JKM, et al. Perioperative Fluid Utilization Variability and Association With Outcomes. Annals of Surgery 263.3 (2016): 502-510.
- Durairaj L and Schmidt GA. Fluid Therapy in Resuscitated Sepsis*. Less is More. Recent Advances in Chest Medicine. 133.1 (2008): 252-263.
- Li, Cheng, et al. Stroke Volume Variation for Prediction of Fluid Responsiveness in Patients Undergoing Gastrointestinal Surgery. International Journal of Medical Sciences. 2013; 10(2): 148-155.
