Freedom from surgical re-intervention at 1 year*
Freedom from reintervention with transcatheter pulmonic valve replacement (TPVR) or valve-in-valve at 1 year*
Available for the treatment of pediatric and adult patients with dysfunctional RVOT conduit or surgical bioprosthetic valve in the pulmonic position.
A less invasive alternative to surgery for patients with a history of pulmonary valve intervention.
Freedom from surgical re-intervention at 1 year*
Freedom from reintervention with transcatheter pulmonic valve replacement (TPVR) or valve-in-valve at 1 year*
The major risks associated with the transcatheter pulmonic valve procedure include death, heart damage potentially requiring surgery, bleeding, blood vessel complications, and irregular heart beat.
All cause death at 1 year† (n=51)^
Endocarditis at 1 year (n=51)^
Valve frame fracture at 1 year (n=51)^
Device success rate (n=53/54)†^
None/trace paravalvular regurgitation at 1 year (n=47)^
^(n=56) COMPASSION S3 trial results using the 20, 23, 26, and 29 mm SAPIEN 3 valve in dysfunctional RVOT conduit or surgical heart valve, valve implant population
† Device success is a composite of
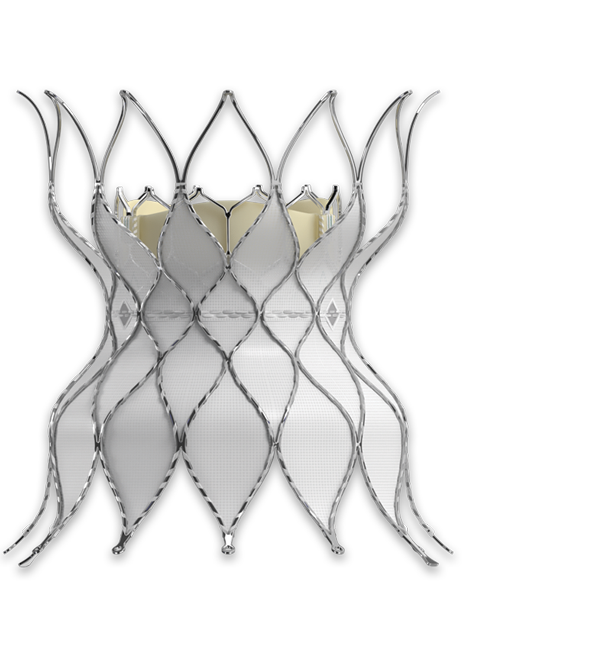
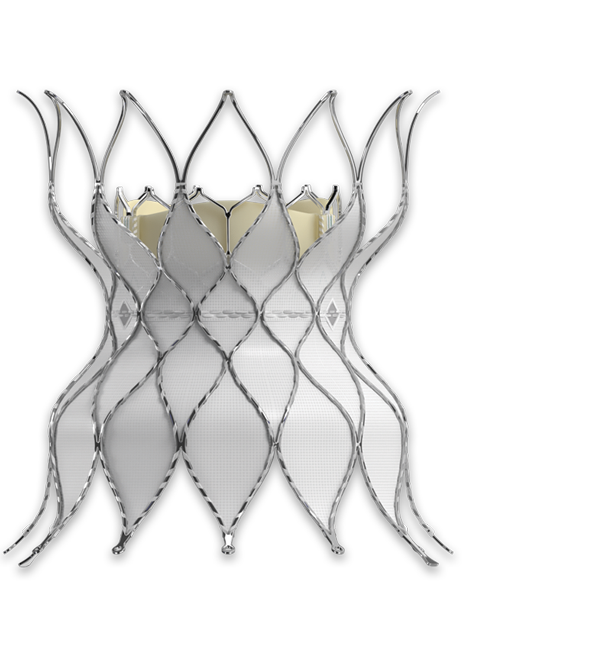
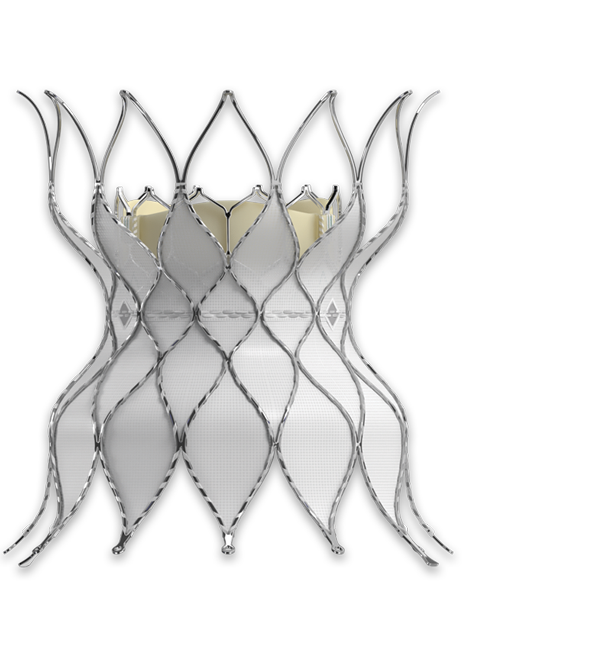
Polyethylene terephthalate (PET) outer skirt is designed to minimize paravalvular leak
Utilizes the same bovine pericardium tissue and processes** as Edwards surgical valves
Enhanced frame geometry for low profile delivery
**Excludes RESILIA tissue
Features of the Edwards Commander delivery system
Features of the Edwards eSheath introducer set
Fewer invasive procedures for more pulmonic patients
Continue meeting the needs of new patient populations with the Alterra adaptive prestent. It allows you to treat more pulmonic patients with severe pulmonary regurgitation with the SAPIEN 3 valve.
Delivering excellent clinical outcomes with sustained performance1
Single Alterra prestent deployed in desired location (n=60)
Single SAPIEN 3 valve deployed in desired location (n=58/60)
Mortality
Endocarditis
Stent fracture requiring reintervention
Reintervention (n=59)
Mild pulmonary regurgitation (n=53)
For more information on transcatheter pulmonic valve replacement with the Edwards SAPIEN 3 valve, visit PulmonaryValveReplacement.com
Download the Edwards SAPIEN 3 transcatheter pulmonic valve patient brochure.
1. Shahanavaz, Shabana Transcatheter Pulmonary Valve Implantation with the Alterra Adaptive Prestent and SAPIEN 3 Transcatheter Heart Valve: Two-Year Outcomes of the Alterra Pivotal Trial; Presented at PICS-AICS 2023, Washington DC.
Indications: The Edwards SAPIEN 3 Transcatheter Heart Valve (THV) System with Edwards Commander Delivery System is indicated for use in the management of pediatric and adult patients who have a clinical indication for intervention on a dysfunctional right ventricular outflow tract (RVOT) conduit or surgical bioprosthetic valve in the pulmonic position with ≥ moderate regurgitation and/or a mean RVOT gradient of ≥ 35 mmHg.
Contraindications: The Edwards SAPIEN 3 THV System with Edwards Commander Delivery System is contraindicated in patients who cannot tolerate an anticoagulation/antiplatelet regimen or who have active bacterial endocarditis or other active infections.
Warnings: The devices are designed, intended, and distributed for single use only. Do not resterilize or reuse the devices. There are no data to support the sterility, nonpyrogenicity, and functionality of the devices after reprocessing. Correct sizing of the valve into the non-compliant RVOT conduit or failing bioprosthesis (landing zone) is essential to minimize risks. Too small of a valve may result in paravalvular leak, migration, or valve embolization; whereas too large of a valve may result in residual gradient (patient-prosthesis mismatch) or RVOT rupture. Accelerated deterioration of the valve may occur in patients with an altered calcium metabolism. Assessment for coronary compression risk prior to valve implantation is essential to prevent the risk of severe patient harm. The physician must verify correct orientation of the valve prior to its implantation; the inflow (outer skirt end) of the valve should be oriented toward the proximal end (handle) of the delivery system to prevent the risk of severe patient harm. Prior to delivery, the valve must remain hydrated at all times and cannot be exposed to solutions other than its shipping storage solution and sterile physiologic rinsing solution. Valve leaflets mishandled or damaged during any part of the procedure will require replacement of the valve. Patients with pre-existing bioprostheses should be carefully assessed prior to implantation of the valve to ensure proper valve positioning and deployment. Do not use the valve if the tamper-evident seal is broken, the storage solution does not completely cover the valve, the temperature indicator has been activated, the valve is damaged, or the expiration date has elapsed. Do not mishandle the delivery system or use it if the packaging or any components are not sterile, have been opened or are damaged (e.g., kinked or stretched), or the expiration date has elapsed. Use of excessive contrast media may lead to renal failure. Measure the patient’s creatinine level prior to the procedure. Contrast media usage should be monitored. Patient injury could occur if the delivery system is not un-flexed prior to removal. Care should be exercised in patients with hypersensitivities to cobalt, nickel, chromium, molybdenum, titanium, manganese, silicon, and/or polymeric materials. The procedure should be conducted under fluoroscopic guidance. Some fluoroscopically guided procedures are associated with a risk of radiation injury to the skin. These injuries may be painful, disfiguring, and long-lasting. It is recommended that all prosthetic heart valve recipients be prophylactically treated for endocarditis to minimize the possibility of prosthetic valve infection. Valve recipients should be maintained on anticoagulant/antiplatelet therapy, except when contraindicated, as determined by their physician. This device has not been tested for use without anticoagulation. Do not add or apply antibiotics to the storage solution, rinse solutions or to the valve.
Precautions: Long-term durability has not been established for the valve. Regular medical follow-up is advised to evaluate valve performance. Glutaraldehyde may cause irritation of the skin, eyes, nose and throat. Avoid prolonged or repeated exposure to, or breathing of, the solution. Use only with adequate ventilation. If skin contact occurs, immediately flush the affected area with water; in the event of contact with eyes, seek immediate medical attention. For more information about glutaraldehyde exposure, refer to the Material Safety Data Sheet available from Edwards Lifesciences. To maintain proper valve leaflet coaptation, do not overinflate the deployment balloon. Appropriate antibiotic prophylaxis is recommended post-procedure in patients at risk for prosthetic valve infection and endocarditis. Patient venous anatomy should be evaluated to prevent the risk of access that would preclude the delivery and deployment of the device. Patient should be heparinized to maintain the ACT at ≥ 250 sec prior to introduction of the delivery system in order to prevent thrombosis. Safety and effectiveness have not been established for patients with the following characteristics/comorbidities: Blood dyscrasias defined as: leukopenia, acute anemia, thrombocytopenia, or history of bleeding diathesis or coagulopathy. A known hypersensitivity or contraindication to aspirin, heparin, ticlopidine (Ticlid™), or clopidogrel (Plavix™), or sensitivity to contrast media, which cannot be adequately premedicated. Positive urine or serum pregnancy test in female subjects of child-bearing potential. Residual mean gradient may be higher in a “THV-in-failing bioprosthesis” configuration than that observed following implantation of the valve inside a native annulus using the same size device. Patients with elevated mean gradient post procedure should be carefully followed. It is important that the manufacturer, model and size of the preexisting bioprosthetic valve be determined, so that the appropriate valve can be implanted and a prosthesis-patient mismatch be avoided. Additionally, pre-procedure imaging modalities must be employed to make as accurate a determination of the inner diameter as possible.
Potential Adverse Events: Potential risks associated with the anesthesia, interventional procedure and imaging include but are not limited to: death; stroke/ transient ischemic attack; respiratory insufficiency or respiratory failure; cardiovascular or vascular injury, such as perforation or damage (dissection) of vessels, myocardium or valvular structures including rupture of the RVOT that may require intervention; pericardial effusion/cardiac tamponade; embolic event: air, calcific material, thrombus, device fragments; infection including incisional site infection, septicemia and endocarditis; myocardial infarction; renal insufficiency or renal failure; conduction system injury, arrhythmia, arteriovenous (AV) fistula; systemic or peripheral nerve injury, systemic or peripheral ischemia, pulmonary edema, pneumothorax, pleural effusion, atelectasis; blood loss requiring transfusion; anemia; radiation injury; electrolyte imbalance; hypertension or hypotension; allergic reaction to anesthesia, contrast media, antithrombotic therapy, device materials; hematoma or ecchymosis, syncope, pain, exercise intolerance or weakness, inflammation; angina; fever; cardiac failure. Potential risks associated with the valve, delivery system and/or accessories include, but may not be limited to, the following: cardiac arrest; cardiogenic shock; coronary flow obstruction/transvalvular flow disturbance, device thrombosis requiring intervention; injury to tricuspid valve; device embolization requiring intervention; device acute migration or malposition requiring intervention; endocarditis; hemolysis / hemolytic anemia; THV dysfunction resulting in pulmonary valve symptoms; mechanical failure of delivery system, and/or accessories; emergent and non-emergent re-intervention; dyspnea.
Indications: The Edwards SAPIEN 3 Transcatheter Pulmonary Valve System with Alterra Adaptive Prestent is indicated for use in the management of pediatric and adult patients with severe pulmonary regurgitation as measured by echocardiography who have a native or surgically-repaired right ventricular outflow tract and are clinically indicated for pulmonary valve replacement.
Contraindications: The Edwards SAPIEN 3 Transcatheter Pulmonary Valve System with Alterra Adaptive Prestent is contraindicated in patients who cannot tolerate an anticoagulation/antiplatelet regimen or who have active bacterial endocarditis or other active infections.
Warnings: The devices are designed, intended, and distributed for single use only. Do not resterilize or reuse the devices. There are no data to support the sterility, nonpyrogenicity, and functionality of the devices after reprocessing. The physician must verify correct orientation of the valve prior to its implantation; the inflow (outer skirt end) of the valve should be oriented towards the proximal end (handle) of the delivery system to prevent the risk of severe patient harm. Prior to delivery, the valve must remain hydrated at all times and cannot be exposed to solutions other than its shipping storage solution and sterile physiologic rinsing solution. Valve leaflets mishandled or damaged during any part of the procedure will require replacement of the valve. Do not use the valve if the tamper evident seal is broken, the storage solution does not completely cover the valve, the temperature indicator has been activated, the valve is damaged, or the expiration date has elapsed. Do not mishandle the delivery system or use it if the packaging or any components are not sterile, have been opened or are damaged (e.g., kinked or stretched), or the expiration date has elapsed. Do not add or apply antibiotics to the storage solution, rinse solutions or to the valve.
Precautions: Long-term durability has not been established for the device. Regular medical follow-up is advised to evaluate device performance. Patients with hypersensitivities to cobalt, nickel, chromium, molybdenum, titanium, manganese, silicon, and/or polymeric materials may have an allergic reaction to these materials. Accelerated deterioration of the valve may occur in patients with an altered calcium metabolism. Assessment for coronary compression risk prior to implantation is recommended. Patient venous anatomy should be evaluated to prevent the risk of access that would preclude the delivery and deployment of the device. Use of excessive contrast media may lead to renal failure. Measure the patient’s creatinine level prior to the procedure. Contrast media usage should be monitored. Fluoroscopically guided procedures are associated with a risk of radiation injury to the skin. Patient radiation dose should be monitored during the procedure. Glutaraldehyde may cause irritation of the skin, eyes, nose and throat. Avoid prolonged or repeated exposure to, or breathing of, the solution. Use only with adequate ventilation. If skin contact occurs, immediately flush the affected area with water; in the event of contact with eyes, seek immediate medical attention. For more information about glutaraldehyde exposure, refer to the Material Safety Data Sheet available from Edwards Lifesciences. Patient should be heparinized to maintain the ACT at ≥ 250 sec prior to introduction of the delivery system in order to prevent thrombosis. To maintain proper valve leaflet coaptation, do not overinflate the deployment balloon. Device recipients should be maintained on anticoagulant/antiplatelet therapy, except when contraindicated, as determined by their physician. This device has not been tested for use without antiplatelet therapy. It is recommended that all device recipients be prophylactically treated for endocarditis to minimize the possibility of prosthetic valve infection. Correct sizing of the prestent into the RVOT is essential to minimize risks such as paravalvular leak, migration, embolization, and/or RVOT rupture. If a prestent fracture is detected with significant loss in valve functionality, reintervention should be considered. Safety and effectiveness have not been established for patients with the following characteristics/comorbidities: blood dyscrasias defined as: leukopenia, acute anemia, thrombocytopenia, or history of bleeding diathesis or coagulopathy; a known hypersensitivity or contraindication to aspirin, heparin, ticlopidine (Ticlid™), or clopidogrel (Plavix™), or sensitivity to contrast media, which cannot be adequately premedicated; positive urine or serum pregnancy test in female patients of childbearing potential.
Potential Adverse Events: Potential risks associated with the anesthesia, interventional procedure, and imaging include but are not limited to death; stroke/transient ischemic attack; respiratory insufficiency or respiratory failure; cardiovascular or vascular injury, such as perforation or damage (dissection) of vessels, myocardium, or valvular structures, including rupture of the RVOT that may require intervention; pericardial effusion/cardiac tamponade; cardiac failure; embolic event: air, calcific material, thrombus, device fragments; infection, including incisional site infection, septicemia, and endocarditis; myocardial infarction; renal insufficiency or renal failure; conduction system injury; arrhythmia; deep vein thrombosis; arteriovenous (AV) fistula; systemic or peripheral nerve injury; systemic or peripheral ischemia; pulmonary edema; pneumothorax; pleural effusion; dyspnea; atelectasis; dislodgement of previously implanted devices (i.e. pacing lead); blood loss requiring transfusion; anemia; radiation injury; electrolyte imbalance; hypertension or hypotension; allergic reaction to anesthesia, contrast media, antithrombotic therapy, device materials; hematoma or ecchymosis; syncope; pain; exercise intolerance or weakness; inflammation; angina; fever. Potential risks, that may or may not require intervention, associated with the valve, prestent, delivery system, and/or accessories include, but may not be limited to, the following: cardiac arrest; cardiogenic shock; coronary flow obstruction/transvalvular flow disturbance; device thrombosis; injury to tricuspid valve; device fracture; device embolization; device acute migration or malposition; endocarditis; chest pain/discomfort; hemolysis/ hemolytic anemia; device penetration/perforation into surrounding vasculature; device dysfunction (regurgitation and/or stenosis); aortic root distortion; embolic events: device fragments; mechanical failure of delivery system, and/or accessories.
Indications: The Edwards crimper is indicated for use in preparing the Edwards SAPIEN 3 Ultra transcatheter heart valve and the Edwards SAPIEN 3 transcatheter heart valve, for implantation.
Contraindications: There are no known contraindications.
Warnings: The device is designed, intended, and distributed for single use only. Do not resterilize or reuse the device. There are no data to support the sterility, nonpyrogenicity, and functionality of the device after reprocessing. Do not mishandle the device. Do not use the device if the packaging or any components are not sterile, have been opened or damaged, or the expiration date has elapsed.
Precautions: For special considerations associated with the use of the Edwards crimper prior to THV implantation, refer to the THV Instructions for Use.
Potential Adverse Events: There are no known potential adverse events associated with the Edwards crimper.
CAUTION: Federal (United States) law restricts these devices to sale by or on the order of a physician.